Sahuarita Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
In Sahuarita, the impact of addiction and mental health challenges is felt across both suburban neighborhoods and rural Pima County communities. While fentanyl and other substances continue to drive record overdose rates, a strong network of treatment providers and recovery supports gives residents meaningful pathways to healing.
In 2023, Pima County reported 532 fatal overdoses, a 7.5% increase and the highest count ever recorded. Middle-aged adults remain especially vulnerable, and access to care often depends on proximity to services. Still, the region’s response is expanding: medical detox and residential programs, outpatient counseling, peer support networks, culturally responsive services, and supportive housing are all part of the local landscape. Mobile crisis teams operate around the clock, while large-scale naloxone distribution has reached thousands of residents each year.
In Arizona, more than 2,200 behavioral health providers serve AHCCCS members, helping to strengthen coverage across Pima County and beyond. The Haven Detox – Arizona provides comprehensive addiction and mental health care serving residents of Sahuarita and surrounding communities. These efforts show that even as the crisis deepens, residents of Sahuarita can turn to a resilient system of care—one designed to meet people where they are and guide them toward recovery.
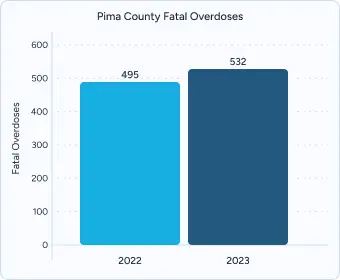
In 2023, Pima County reported 532 fatal overdoses, a 7.5 percent increase from 495 in 2022 and the highest count on record. Toxicology reviews show methamphetamine present in 77.3 percent of cases and fentanyl in 60 percent, compared with 36.7 percent involving prescription opioids. By contrast, Arizona’s statewide opioid mortality rate remained relatively stable at 25.6 deaths per 100,000 residents.
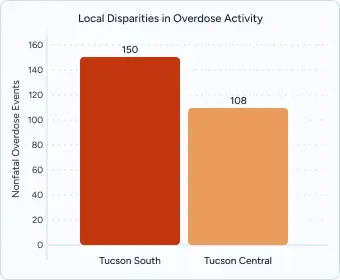
Overdose activity varies widely across the county. Tucson South recorded 150 nonfatal overdose events in 2023, followed by Tucson Central with 108. Meanwhile, suburban areas such as Sahuarita and Green Valley saw significantly lower rates. Across Arizona, urban areas, including Phoenix’s Central City Village, Mesa West, and Buckeye, also reported elevated activity.
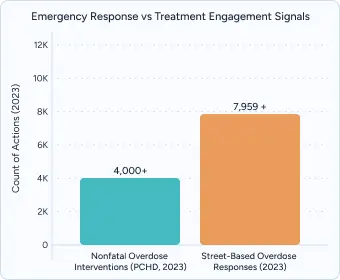
Even with expanded outreach, treatment enrollment remains a challenge. In 2023, the Pima County Health Department completed more than 4,000 nonfatal overdose interventions, while street-based teams responded to over 7,959 suspected overdoses. Yet state data show a decline in formal substance use treatment admissions compared with prior years—underscoring the need for better navigation, reduced barriers, and stronger referral pathways.
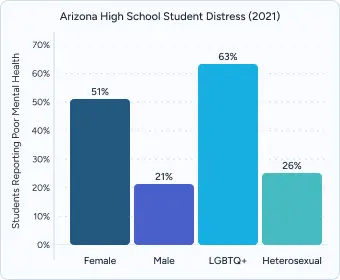
In 2021, about 4 in 10 Arizona high school students reported poor mental health during the COVID-19 period. The burden was not evenly shared: 51 percent of female students and 63 percent of LGBTQ+ youth reported high levels of distress, compared with 21 percent of males and 26 percent of heterosexual peers. That same year, 23 percent of students seriously considered suicide, 20 percent made a plan, and 10 percent reported an attempt.
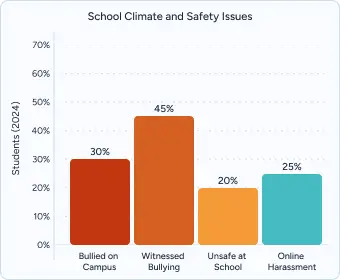
Pima County data show that school climate plays a significant role in youth well-being. In 2024, nearly 30 percent of students said they were bullied on campus, 45 percent witnessed bullying, and 20 percent reported feeling unsafe at school. About one in four experienced online harassment in the prior year—issues that directly affect students in Sahuarita and surrounding communities.
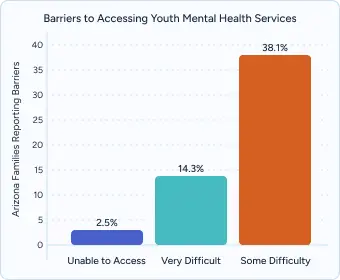
Even when symptoms are recognized, families often struggle to find help. Statewide analyses show 38.1 percent of Arizona families reported “some difficulty” obtaining youth mental health services, 14.3 percent described it as “very difficult,” and 2.5 percent were unable to get care at all. These access gaps are especially concerning given that 36.8 percent of Arizona high schoolers report living with someone who had an alcohol or drug problem, increasing both stress and vulnerability.

Sahuarita residents have access to a growing network of treatment providers that bridge critical gaps across southern Arizona.
Pima County’s Crisis Mobile Team (CMT) system responds anywhere in the county (including rural or suburban areas) for voluntary or involuntary evaluations, critical stress debriefings, and connects people with follow-up care.
Transportation remains important in the treatment infrastructure. Sun Tran routes and regional transit options link Sahuarita to Tucson’s behavioral health corridor, while paratransit services provide door-to-door access to outpatient clinics and community centers. For those covered under AHCCCS, specialized medical transportation benefits ensure individuals with disabilities or mobility challenges can reach appointments without barriers.
Despite these resources, southern Arizona continues to face a shortage of licensed behavioral health professionals. Pima County reports fewer providers per capita compared to the national average, especially in suburban and rural areas like Sahuarita. This shortage can lead to longer wait times and greater reliance on mobile crisis teams, peer specialists, and nonprofit organizations to meet urgent needs. Expanding the workforce remains a key priority for improving long-term access to consistent, high-quality care.
AHCCCS provides medically necessary care for eligible Sahuarita residents, including medical detox, outpatient programs, residential treatment, crisis stabilization, and medication-assisted treatment (MAT) with buprenorphine, methadone, or naltrexone. Coverage extends to adults up to 138% of the federal poverty level, with no-cost access to 24/7 crisis services.
This integrated plan combines physical and behavioral health care, ensuring coordinated services such as outpatient therapy, peer recovery support, case management, and crisis intervention. Enrollment is available online or by calling 1-888-788-4408, with multilingual support for Spanish-speaking residents.
AIHP provides Native American residents access to culturally responsive care, covering behavioral health and addiction services across Arizona. Services include crisis stabilization, outpatient therapy, and linkage to peer recovery resources that respect tribal cultural traditions.
Pima County collaborates with local community health centers and nonprofits to extend treatment access for uninsured residents. Supports include sliding-scale fees, naloxone distribution, and navigation services for families seeking treatment referrals.
Private and community-based providers in Sahuarita offer rapid assessments, insurance verification, and evidence-based therapies like CBT, DBT, and trauma-informed care. Many programs also provide holistic supports such as nutrition counseling, yoga, and fitness programs to enhance recovery.
Behavioral health services are available through hospitals, outpatient clinics, and nonprofit organizations. Programs focus on depression, trauma, dual-diagnosis treatment, and crisis stabilization. Culturally responsive supports, including bilingual Spanish-speaking clinicians and family counseling, help bridge care gaps in Sahuarita and surrounding communities.
HOPE, Inc. Recovery Center in Tucson (1200 N. Country Club Rd.) provides free peer-led recovery support, specialized trauma groups, and sober social events with bilingual facilitation. The center features 24/7 crisis warm line access and weekend hours designed for working professionals.
Most Sahuarita facilities offer same-day comprehensive evaluations, followed by personalized treatment recommendations. COPE Community Services emphasizes warm handoffs from crisis stabilization or walk-in behavioral health services to outpatient care and peer support programs, helping individuals stay connected after a crisis. Providers often coordinate with families, schools, and referral agencies to support engagement and readiness for care.
NAMI Southern Arizona, located at 6122 E. 22nd St. in Tucson, delivers family education programs, peer-led support circles, and advocacy training with a strong focus on mental health awareness. Programming is free of charge and includes evening and weekend options for caregivers balancing multiple responsibilities.
Certified sober living homes across Southern Arizona operate under the oversight of the Arizona Recovery Housing Association (AzRHA), which enforces standards consistent with the National Alliance of Recovery Residences (NARR).
Recovery Living Solutions, a NARR Level 2 residence, provides 24-hour on-site support, secure keyless entry, Wi-Fi, laundry facilities, and dedicated parking. Residents are expected to participate in weekly drug screenings, attend 12-step meetings, rotate household chores, and observe a 10 PM weeknight curfew.
Desert Recovery Residences maintains Level 3 accreditation with a higher level of clinical coordination. The program integrates structured recovery programming with access to community kitchens, secure entry systems, and transportation assistance. Weekly house meetings and sobriety checks are required to support accountability and progress.
The Southern Arizona Intergroup Service Office manages more than 200 weekly recovery meetings throughout Pima County. It partners with mobile apps to provide up-to-date schedules and operates a 24/7 hotline at (520) 881-8381 for individuals seeking immediate support.
Spanish-speaking recovery groups serve Hispanic and Latino families in Tucson and Green Valley, with programming led by native-language facilitators. Grupo Hispano networks ensure daily meeting options and integrate family-centered programming.
Additional recovery meetings are hosted in community centers and treatment facilities with evening schedules that accommodate older adults and professional life. Many programs partner with the University of Arizona to offer additional outreach and maintain active online communities through smartphone apps.
A comprehensive assessment should address both substance use and mental health conditions. Look for programs that screen for trauma, evaluate family supports, and use the results to build a personalized care plan.
Choosing a program with these elements increases the likelihood of safe stabilization, meaningful engagement, and lasting recovery.
Aftercare Coordination should begin during active treatment and connect clients with outpatient therapy, peer-led support groups, and transitional housing through warm handoffs and ongoing community partnerships. Programs maintaining alumni networks and providing continuing care coordination demonstrate commitment to sustained recovery outcomes.
Family Engagement and Support improves treatment outcomes by involving loved ones through multi-family therapy sessions and educational workshops about addiction and recovery. Many programs offer culturally tailored family programming with Spanish-language and faith-based offerings for diverse community needs.
Evidence-based therapies anchor care and build lasting recovery. Programs combine trauma treatment with approaches for co-occurring mental health conditions and substance use. When clinically appropriate, services may include Eye Movement Desensitization and Reprocessing (EMDR), trauma-focused CBT, somatic therapies, and neurofeedback—delivered by clinicians who maintain specialized training and ongoing continuing education.
Alumni networks and continuing care keep support going well beyond discharge. Many programs offer lifelong alumni connections, regular groups and workshops, and digital peer forums that link graduates across Arizona. Step-down options (PHP/IOP), relapse-prevention planning, and family resources help people navigate challenges that can arise months or years later.
Insurance coordination and advocacy make care easier to access. Dedicated teams verify benefits, explain coverage, and help with prior authorizations. When available, financial counselors discuss sliding-scale options and coordinate referrals so individuals can move smoothly between levels of care without gaps.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Begin Your Recovery Journey with immediate access to professional assessment and support services.
Insurance and Benefits Verification streamlines access through comprehensive coverage review and cost estimation assistance, with specialist staff completing verification within 24-48 hours for most major insurance plans.
Assessment and Intake Services provide same-day psychological evaluations and next-day treatment placement, with clinical staff available for immediate assessment and specialized intake coordinators minimizing administrative delays.
Most programs schedule an initial assessment within 48 hours, then connect you with a therapist based on your needs and preferences.
Yes, Arizona Medicaid covers individual and group therapy with no copayments; check your specific plan for provider network details and eligibility criteria.
Yes. Many community centers offer bilingual and Spanish-language peer-support meetings, with native speakers facilitating specialized cultural programming.
Several nonprofit clinics provide sliding-scale fees and grant-funded treatment; inquire about financial assistance and state-funded programs when contacting intake offices.
Some programs partner with AHCCCS transportation benefits and regional transit to offer free or low-cost transportation vouchers for treatment clients.
Crisis hotlines and mobile response teams operate 24/7—call the Arizona statewide crisis line at 1-844-534-4673 for immediate mental health or substance-related support.
Yes. Family peer specialists offer confidential coaching and referrals to Al-Anon, family therapy, and professional intervention services throughout Pima County.
Look for centers offering Spanish-language groups, Native American healing circles, LGBTQ+-affirming programming, and faith-based support tailored to diverse community needs.
Yes. Many organizations run college outreach programs, peer-led support circles, and specialized workshops designed for adults aged 18-25 in recovery.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!