Opiates, sometimes known as “opiate painkillers,” include prescription medications such as Codeine, Dilaudid, and Tramadol. Those who take these medications in higher quantities or for longer durations than advised run a greater risk of developing physical dependency.
Those who develop a physical dependence on opioid painkillers will feel compelled to continue taking them to function normally. If they abruptly stop taking medicine, they will experience painful withdrawal symptoms.
Withdrawal happens when an individual suddenly quits using a substance or reduces their dosage. The withdrawal symptoms can vary quite a bit depending on the type of painkiller being misused, the individual’s built tolerance to the drug, the length of their addiction, whether they abused multiple substances, and their mental and medical history. Most withdrawal symptoms are flu-like, including fever, sweating, and vomiting.
While withdrawal symptoms are often not life-threatening, they can cause a great deal of physical and mental distress to the individual experiencing them. Due to the severity of withdrawal symptoms, individuals attempting to quit drugs on their own may relapse to escape the withdrawal process. However, the pattern of stopping and restarting drug use might make it more challenging to quit in the future because the cycle can develop into uncontrolled habits of abuse.
Symptoms of Opioid Withdrawal
The degree of withdrawal you go through will determine the symptoms you encounter. Several factors also determine the length of time that someone will suffer withdrawal symptoms.
Because of this, everyone’s experience of opiate withdrawal is unique. However, the course of symptoms often follows a timeframe.
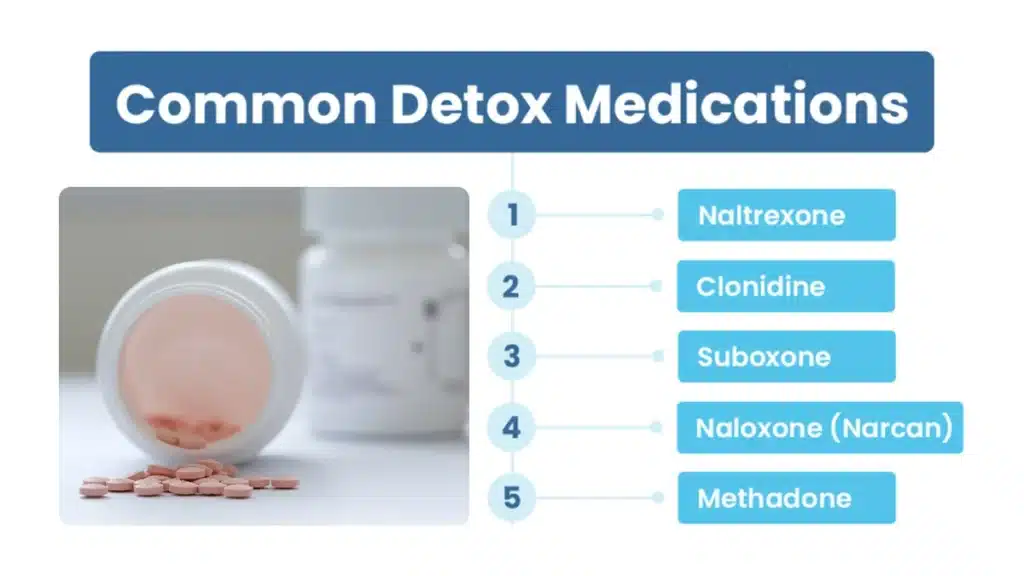
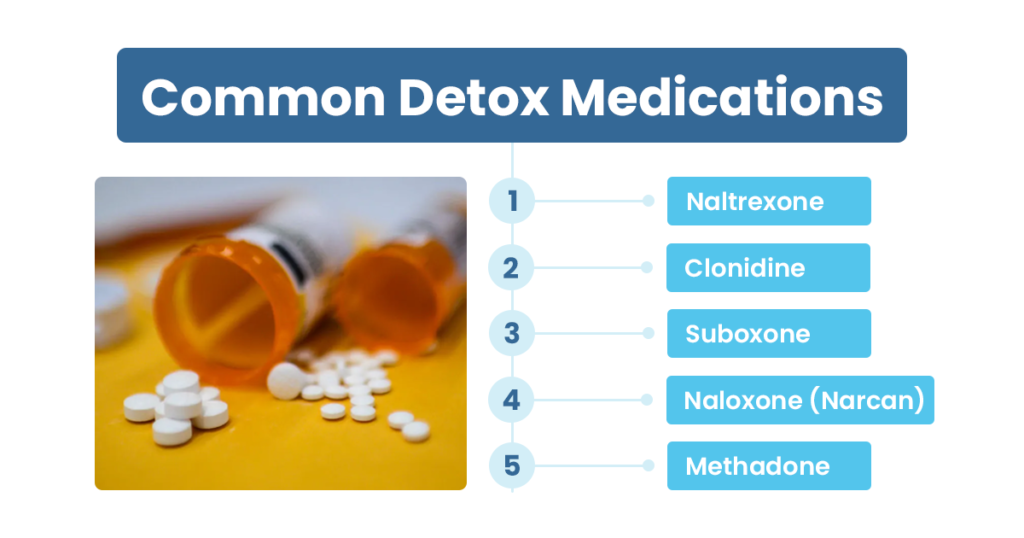
Medications Used in Opiate Detoxification
During the detoxification process, doctors often recommend medications. These medications help treat long-term withdrawal-related problems such as drug cravings. A physician will progressively reduce the dosage of these drugs over time until the patient is free of acute withdrawal symptoms.
Medications may continue to be prescribed while the patient receives treatment in an inpatient rehab program. Below are some of the most common drugs used during opiate detox:
Naltrexone
Naltrexone is commonly prescribed for the treatment of opioid dependence. By blocking the adverse effects of opioids, the medication lowers the drug-induced cravings. It should be part of an entire rehabilitation program, which may include counseling, support groups, and other treatment methods suggested by your doctor or certified therapist.
If you are physically dependent on opioids, taking naltrexone will cause withdrawal symptoms. To lessen the risk of withdrawal, it is essential to abstain from opioids for at least 7 to 10 days before starting taking naltrexone. However, the duration will vary from person to person based on the kind of opioid addiction, the dose, and the duration of the addiction.
Recovery from opioid addiction requires time and dedication since it is not a quick process. However, with the help of medication such as naltrexone and a variety of treatment options, you will have constant support.
Clonidine
Clonidine belongs to the drug class known as Antihypertensive. It is widely used as a treatment for opioid withdrawal symptoms. Clonidine inhibits brain chemicals that stimulate sympathetic nervous system activity.
This decreases unpleasant withdrawal symptoms such as sweating, hot flushes, watery eyes, and restlessness. Additionally, clonidine has been shown to reduce anxiety and shorten the detoxification process.
Combining medication with inpatient or outpatient therapy, support groups, and professional counseling increases the likelihood of recovery. Most approved treatment centers like The Haven provide a recovery plan that includes multiple facets of treatment.
Naloxone (Narcan)
Naloxone, which comes under the brand name Narcan, is a medication used to counteract the damaging consequences of an opioid overdose. Opioids include heroin, hydrocodone, morphine, oxycodone, and others. An opioid overdose may be exceedingly detrimental to a person’s health if not handled quickly.
In response to the rising number of opioid-related deaths in the United States, naloxone provides a lifesaving treatment until emergency medical professionals arrive. The medication should only be administered if a person’s system contains opioids.
Narcan does not counteract other medicines and should not be distributed to persons whose systems do not include opioids. Although Narcan helps reverse the effects of an opioid overdose, it should not be administered to persons actively taking opioids. If you are battling an opioid addiction, contact a treatment provider to be referred to a treatment facility in your area.
Suboxone
Suboxone is a prescription drug used to treat opioid addiction, whether illegal or prescribed. It comprises buprenorphine and naloxone. As a partial opioid agonist, buprenorphine inhibits opiate receptors and lowers a person’s cravings. The second component, naloxone, is used to counteract the effects of opioids.
Together, these medications reduce the withdrawal symptoms associated with opioid dependence. Suboxone may be administered by your doctor, unlike other opioid replacement drugs that require a prescription from a specialist treatment center. Suboxone is frequently used at the start of treatment and during treatment and recovery. Your physician or addiction counselor can assist you in developing an individualized treatment plan.
Suboxone can help you manage the withdrawal symptoms associated with opioid cessation, but finding a complete treatment program is crucial. Counseling and therapy can help you tackle the underlying cause of your opioid abuse and develop new coping mechanisms for pain and stress.
Methadone
Methadone was commonly used in detoxification settings, but buprenorphine has mostly supplanted it. Typically, it is prescribed to assist people in gradually withdrawing from the drug to which they were first addicted. Methadone, a long-acting opioid, is most successful as a long-term treatment for people with chronic opiate addiction.
Over-the-Counter Medications For Opioid Withdrawal
It is often recommended to use over-the-counter medications, but this should only be done under medical supervision and as part of an established treatment plan.
Some opiate withdrawal symptoms are common and can be relieved with over-the-counter drugs.
For example, loperamide, a non-prescription diarrhea medication, can be used to treat diarrhea that occasionally develops with opiate withdrawal. Other over-the-counter medications for opiate withdrawal symptoms that might be used while receiving treatment from a qualified treatment facility include:
- Anti-nausea formulations like Pepto Bismol
- Natural sleep supplements such as Valerian root, Melatonin
- Non-steroidal anti-inflammatory drugs (NSAIDs), like ibuprofen, naproxen, and aspirin
- Topical analgesics such as Tiger Balm or Ben Gay
Because every over-the-counter medication has the potential to interact with other drugs, a doctor can assist in ensuring that the patient avoids anything that could interfere with other medicines recommended to treat the addiction.
Frequently Asked Questions (FAQs)
How can I counteract the effects of opiates?
The medication naloxone (Narcan®) is used to treat overdoses immediately. Naloxone can reverse the symptoms of an opioid overdose if administered quickly.
Which substance has the most severe withdrawal symptoms?
Methamphetamine, heroin, opiates, and other powerful drugs can cause some of the most severe cases of potentially fatal drug withdrawal symptoms. A person may harm oneself or others due to extreme delusion and hallucinations during withdrawal.
What can I take to stop withdrawal symptoms?
– Methadone alleviates withdrawal symptoms and facilitates the detoxification process.
– Buprenorphine can reduce withdrawal symptoms and decrease the detox phase.
– Clonidine can treat anxiety, agitation, and muscular pains.
What drugs are hard to withdraw from?
Addictive drugs induce severe withdrawal symptoms and cravings, making it difficult to quit using them. Some of the hardest drugs to withdraw from are:
– Methamphetamine & Crystal Meth
– Nicotine
– Heroin and prescription painkillers
– Cocaine
– Alcohol
– Benzodiazepines
What is a rapid opiate detox program? Does it work?
During a rapid detox treatment, a patient is placed under anesthesia for four to six hours while opioid antagonist medications (such as naltrexone) “kick out” the opioid substances, such as heroin or prescription opioids.
Multiple research conducted by the National Institute on Drug Abuse (NIDA) demonstrates that this method is ineffective for sustaining recovery. Treatment providers and doctors do not promote rapid detox, which is not considered an efficient kind of detox.
Begin Your Recovery Today with The Haven
The process of tapering off opioids requires time and commitment. Withdrawal symptoms are uncomfortable, but they will lessen gradually over time, making the recovery much smoother. The Haven treatment center provides the appropriate therapies to help you avoid many of these symptoms and prevent relapse in the future.
Our medical team of expert doctors and therapists provides effective treatment for opiate detox and understands the discomfort of withdrawal symptoms. They can offer further valuable tips and tricks to assist with opiate withdrawal.
For further information, contact us at (561) 328-8627 today!