Arkansas Addiction and Mental Health Treatment Resource Guide
Arkansas is grappling with a severe behavioral health crisis. In 2024, 391 people died from drug overdoses—a 24% decline from 2023, yet the state still ranks second nationally for opioid prescribing at 72.2 prescriptions per 100 residents. Substance use treatment remains elusive: of the roughly 20% of Arkansans needing care, only 5.9% received it—leaving 70.5% without support.
Mental health needs are equally pressing. 457,000 adults live with a mental health condition, and 65.7% of youth aged 12–17 with depression received no care in the past year. Workforce shortages exacerbate these gaps: 1.43 million Arkansans reside in areas lacking adequate mental health professionals, and the state meets just 33.7% of its provider needs.
These challenges underscore the necessity of accessible, evidence-based services. By navigating available state, community, and Medicaid-funded programs—and advocating for expanded capacity—individuals and families can connect with the lifesaving care and support they deserve.
Need Professional Treatment Today? The Haven Detox – Arkansas delivers rapid admission, private treatment, around-the-clock medical monitoring for safer withdrawal, and integrated behavioral health care to address co-occurring disorders.

388 overdose deaths in 2024 (provisional data), down 24% from 516 deaths in 2023
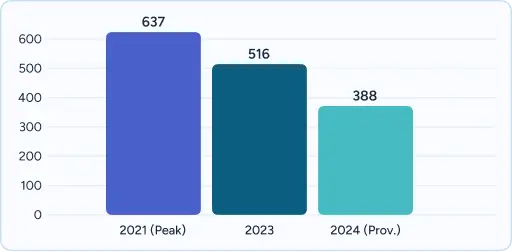
Peak overdose deaths of 637 occurred in 2021, representing the state’s highest on record
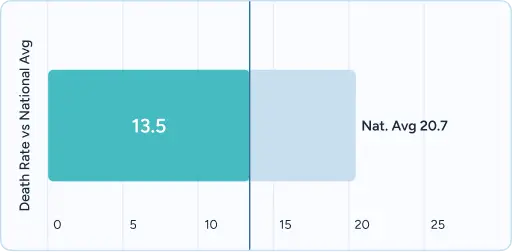
Arkansas’s death rate of 13.5 per 100,000 residents is 34.78% below the national average
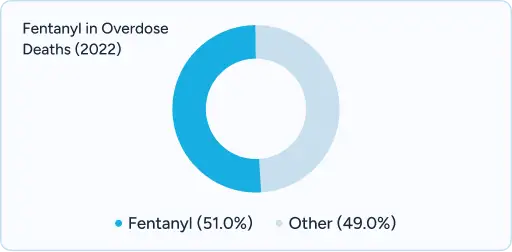
Fentanyl involved in 51% of total overdose deaths in 2022
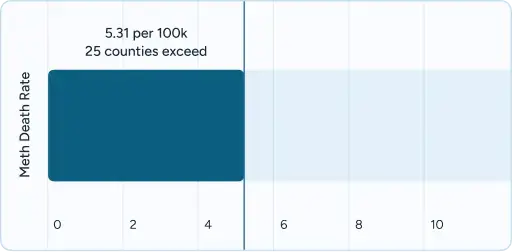
Methamphetamine death rate of 5.31 per 100,000 with 25 counties exceeding this rate
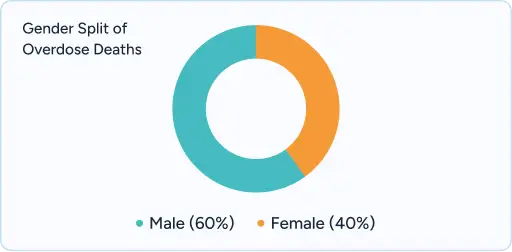
Males account for ~60% of overdose deaths with the highest rates among ages 25-44
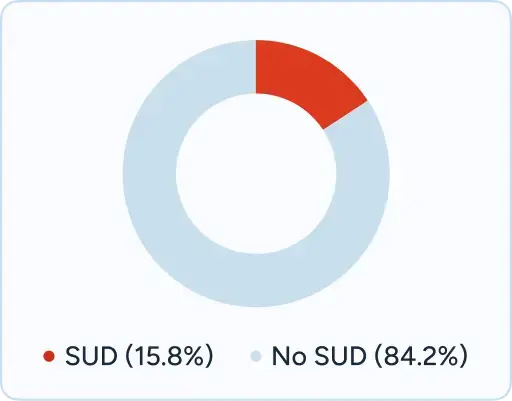
15.8% of individuals aged 18 and older had substance use disorder in recent assessments
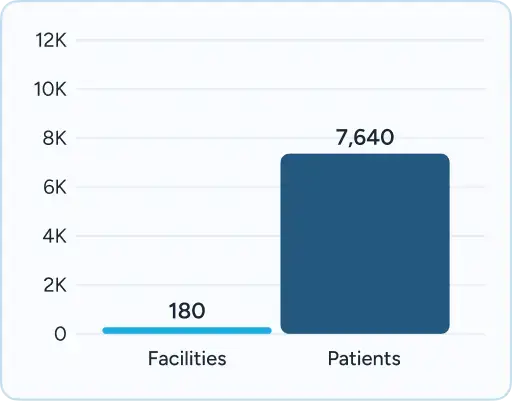
180 substance abuse treatment facilities operating statewide serving 7,640 patients annually
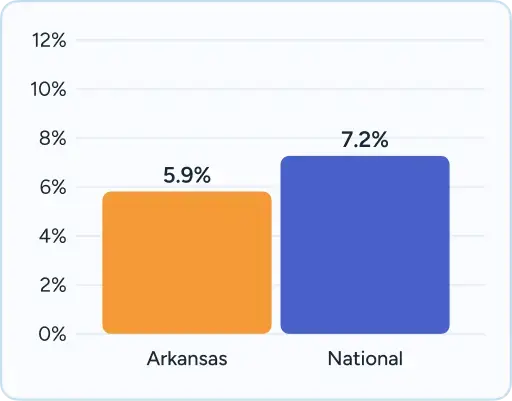
Only 5.9% of Arkansans with substance use disorders received specialty treatment in 2022, below the 7.2% national average
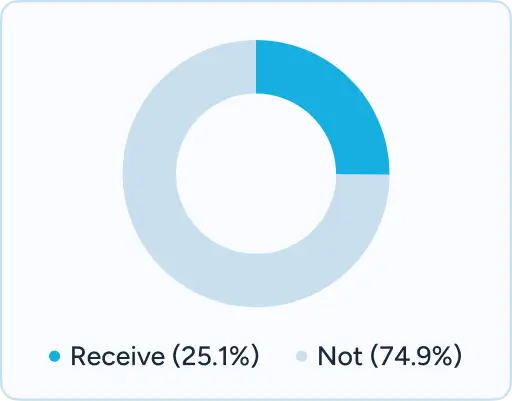
74.93% treatment gap exists with those needing treatment not receiving it
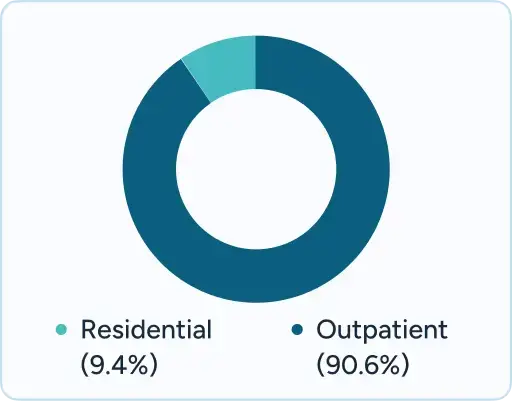
Treatment admissions have been stable with 90.6% outpatient and 9.4% residential services

Arkansas has emerged as a premier treatment destination for individuals seeking comprehensive addiction and mental health services throughout the Mid-South region. The state’s central location provides accessible care for residents of neighboring states, including Tennessee, Mississippi, Louisiana, Texas, Missouri, and Oklahoma, with major treatment centers concentrated in Little Rock, Fort Smith, Jonesboro, Hot Springs, and Fayetteville.
The state’s excellent transportation infrastructure enhances accessibility, with Interstate 40 running east-west and Interstate 55 connecting north-south, making quality treatment facilities reachable from across the region. Arkansas treatment centers serve approximately 20-25% out-of-state patients, particularly those seeking specialized dual diagnosis care and medication-assisted treatment programs.
Arkansas offers a comprehensive continuum of care from emergency intervention through long-term recovery support. The state’s 180 treatment facilities provide services ranging from outpatient counseling to residential programs, with specialized tracks for professionals, adolescents, and individuals with co-occurring disorders. Major medical centers like UAMS in Little Rock and regional health systems provide medically supervised detoxification and psychiatric stabilization services.
The therapeutic environment benefits from Arkansas’s natural beauty and significantly lower cost of living compared to neighboring states, creating an ideal setting for recovery. Treatment centers utilize the state’s outdoor recreation opportunities as part of holistic healing approaches, while maintaining proximity to urban medical resources and support services. This combination of accessibility, affordability, and comprehensive care has established Arkansas as a regional leader in behavioral health treatment.

Understanding insurance coverage for behavioral health services can feel overwhelming, especially when facing a mental health crisis or addiction emergency. Insurance policies often contain complex language about prior authorizations, network restrictions, and medical necessity requirements that can delay or prevent access to life-saving care. Professional treatment centers in Arkansas employ dedicated insurance specialists who verify benefits, obtain necessary pre-authorizations, and work directly with insurance companies to maximize coverage while minimizing financial barriers for individuals and families.
While Arkansas offers excellent public resources, professional treatment facilities provide distinct advantages when immediate care is needed:
Every person struggling with addiction or mental health challenges in Arkansas deserves compassionate, professional care that addresses their unique needs and circumstances. Professional treatment centers provide the medical expertise, therapeutic support, and comprehensive resources necessary to build lasting recovery and mental wellness. With 391 Arkansans losing their lives to overdoses in 2024 and thousands more struggling with untreated mental health conditions, seeking immediate professional help can be the life-saving decision that transforms not just individual lives, but entire families and communities throughout the Natural State.
Verify benefits and understand your treatment options
If you or a loved one is experiencing a mental health or substance use crisis, help is available right now:
Private treatment facilities typically offer same-day or next-day admission for individuals with insurance coverage or private pay arrangements. State-funded Community Mental Health Centers may have waiting periods of several days to weeks depending on the level of care needed and current capacity. Emergency situations receive priority placement through crisis stabilization units available 24/7 in Little Rock, Fort Smith, and Jonesboro, with mobile crisis teams providing immediate assessment and referral services.
Arkansas Medicaid and ARKids First cover substance abuse treatment services and mental health care at enrolled private facilities. Coverage includes outpatient counseling, intensive outpatient programs, medication-assisted treatment, and medically necessary residential treatment. Private facilities must be enrolled Arkansas Medicaid providers, and some services may require prior authorization. Recent policy changes in 2024 improved reimbursement rates for behavioral health services to 80-100% of Medicare rates.
Out-of-state residents can access treatment in Arkansas, with insurance coverage varying by plan and state. Many Arkansas facilities accept out-of-state Medicaid through interstate compacts, and private insurance typically covers services regardless of state boundaries. Crisis services through 988 and emergency departments are available to anyone, while ongoing treatment may require verification of coverage or private pay arrangements. Approximately 20-25% of Arkansas treatment center patients come from neighboring states.
Arkansas follows integrated treatment models where mental health and substance use disorders are addressed simultaneously by the same treatment team. The state’s Community Mental Health Centers and private facilities provide dual diagnosis treatment combining psychiatric medication management, individual and group therapy, and specialized interventions for trauma and other co-occurring conditions. The Arkansas Medicaid program covers integrated services, and the state has invested in training providers on co-occurring disorder treatment approaches.
Arkansas law allows involuntary commitment for individuals who are “homicidal, suicidal, or gravely disabled” due to mental illness or substance use. Family members, healthcare providers, or concerned individuals can file a petition with the circuit court under Arkansas Code § 20-64-815, which requires medical evaluation and judicial review. The process includes due process protections and typically results in a 21-day initial commitment period for substance use disorders, with longer periods possible for mental health commitments based on clinical assessment.
Most professional treatment centers in Arkansas offer alumni services and readmission policies for graduates who experience relapse. Community support through peer recovery organizations like the Wolfe Street Foundation, ongoing outpatient therapy through Community Mental Health Centers, and medication-assisted treatment help prevent relapse. When relapse occurs, individuals can typically re-enter treatment quickly, often at a different level of care based on current needs, with many facilities providing rapid readmission within 24-48 hours.
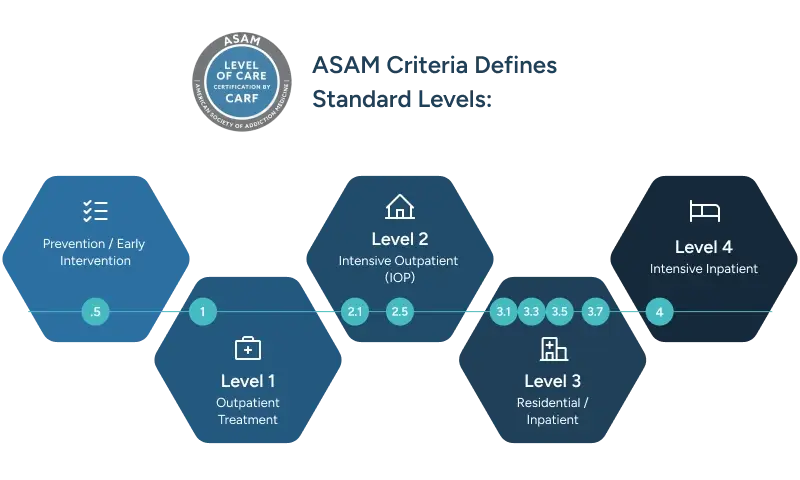
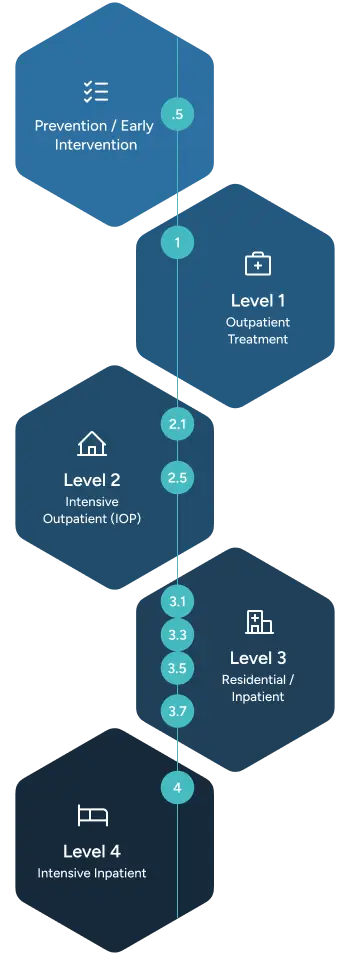
Treatment duration varies based on individual needs and level of care required. Medical detoxification typically lasts 3-7 days in Arkansas facilities, residential treatment programs range from 30-90 days, and outpatient therapy may continue for months or years. Arkansas facilities follow American Society of Addiction Medicine (ASAM) criteria to determine appropriate length of stay based on severity of addiction, co-occurring conditions, and social support factors, with insurance coverage typically determining duration limits.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!