
Get Help Today 24/7

If you or someone you love has been diagnosed with bipolar disorder, you’ve probably wondered, “Is this something I inherited?” or “Could I pass this on to my children?”
The answer is: bipolar disorder does have a genetic component, but the full picture is more complex than a simple “yes” or “no.” Let’s take a closer look at what we know about the genetic and environmental factors that influence bipolar disorder.
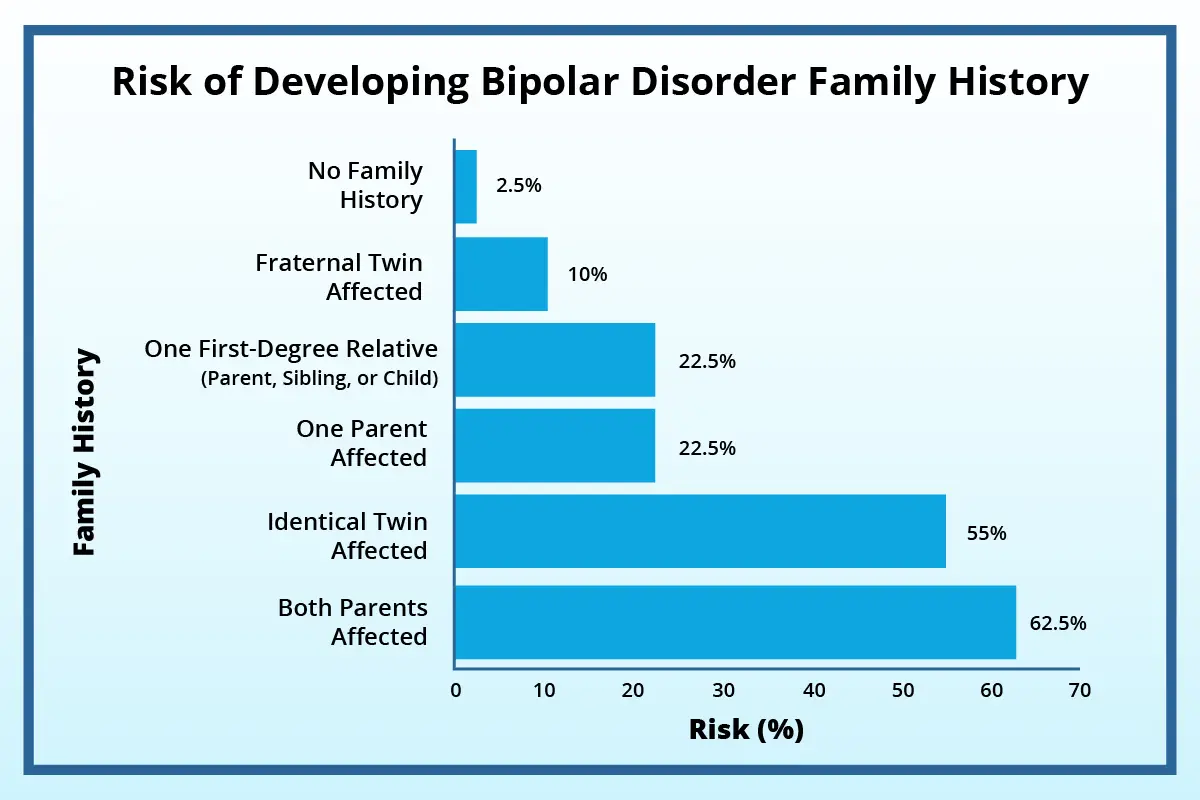
Bipolar disorder tends to run in families—similar to how you might inherit your mom’s eye color or your dad’s height. Research has found clear genetic links, especially among immediate family members.
But here’s the important part: having a genetic predisposition doesn’t guarantee you’ll develop the condition. Most children with a family history of bipolar disorder will not go on to develop it.
Bipolar disorder is associated with irregularities in neurotransmitters—chemical messengers that help brain cells communicate. When these messengers don’t work properly, it can lead to extreme shifts in mood, energy, and behavior.
Brain areas that regulate emotion, sleep, energy, and decision-making don’t always “sync up” in individuals with bipolar disorder.
Scientists have identified several genes that contribute to bipolar disorder. Think of these genes as a team of players—each one influencing how your brain functions and responds to internal and external changes. Understanding these genes helps researchers work toward more targeted treatments.
This gene manages calcium flow in brain cells, which is essential for emotional regulation and memory. Calcium channels are like “gates” that allow messaging between brain cells.
ANK3 organizes where electrical impulses begin in brain cells. It’s like the blueprint for your brain’s internal wiring.
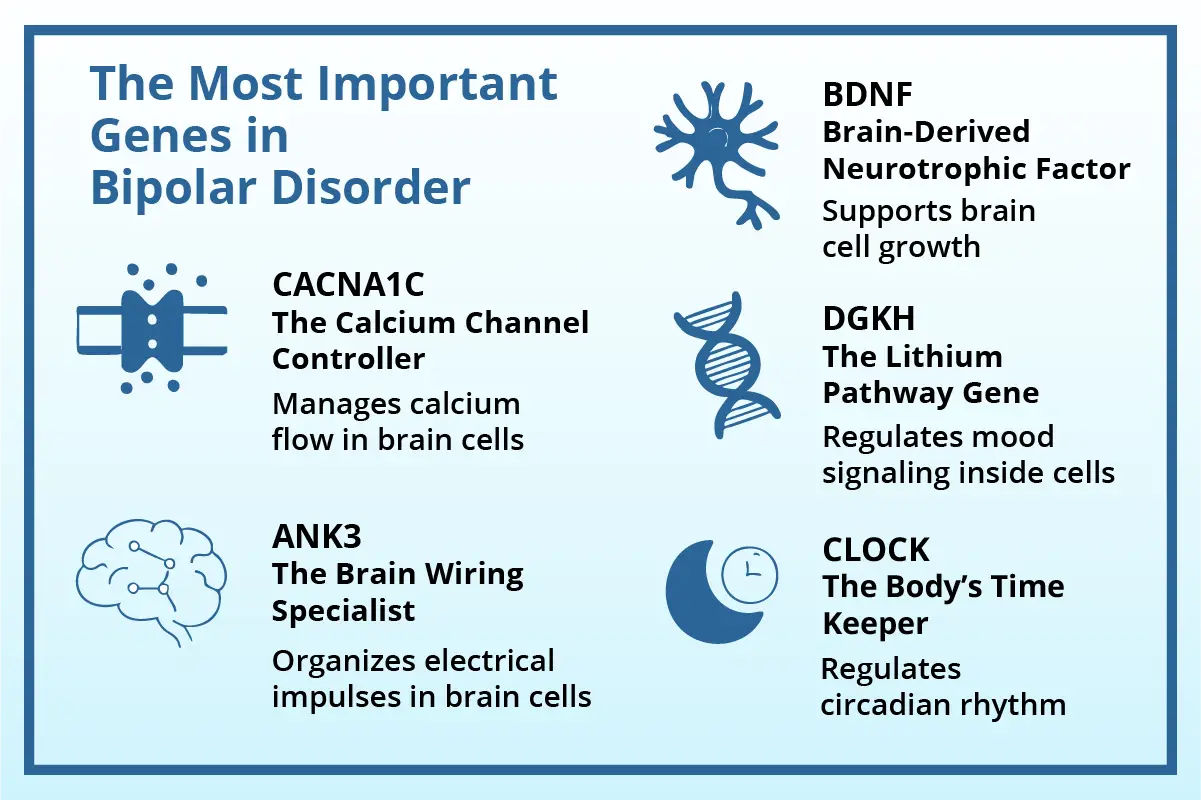
This gene regulates your circadian rhythm—your body’s 24-hour internal clock controlling sleep, mood, and energy.
This gene helps regulate enzymes in the phosphoinositide pathway, which lithium is known to affect. It plays a role in mood signaling inside cells.
BDNF supports brain cell growth, survival, and synaptic plasticity—it’s often called “brain fertilizer.”
These genetic insights reveal how specific genes—from lithium pathways to circadian rhythms—shape mood regulation, treatment response, and recovery in bipolar disorder, opening the door to more precise, personalized mental health care.
Although we’ve made major discoveries, mental health genetics is incredibly complex. Here’s why targeted medications are still rare:
However, this research is shaping the next generation of psychiatric care—from personalized medication regimens to early screening tools. At The Haven Detox, we stay informed on these innovations to better support our clients.
While genetics play a significant role, environmental factors also influence the onset and severity of bipolar disorder. Think of genes as setting the stage—life experiences determine the script.
Emotional or physical trauma early in life may increase risk and severity of symptoms.
Events like a job loss, divorce, or even a major life change (like starting college) can act as triggers in those genetically predisposed.
Alcohol and drug use can trigger bipolar episodes and worsen existing symptoms. Around 60% of people with bipolar disorder have a history of substance abuse.
Changes in sleep patterns—either too little or too much—can trigger manic or depressive episodes.
Understanding how these environmental factors interact with genetic vulnerability gives a fuller picture of bipolar disorder’s development and management.
At this time, there isn’t a genetic test that can diagnose bipolar disorder. While scientists have learned a lot about the genes involved, the condition is too complex for a simple test to give a clear answer.
However, for those already diagnosed, there’s an exciting development in genetic testing for medication response: pharmacogenomic testing.
GeneSight is a popular pharmacogenomic test that helps predict how your body will respond to psychiatric medications.
Think of genetic risk factors as increasing sensitivity, not sealing your fate. With early intervention, healthy lifestyle choices, and personalized treatment, most people with bipolar disorder can lead fulfilling, stable lives.
Moreover, the fact that many genes overlap with other conditions (like depression or schizophrenia) is promising—it means treatments targeting one condition could potentially help others too.
Understanding the biological roots of bipolar disorder also helps reduce stigma. These are real, measurable brain-based conditions—not moral failings or personal weaknesses.
Bipolar disorder can be overwhelming, but help is available—and effective.
The good news is that with proper treatment – including medication and therapy – people with bipolar disorder can live happy, successful lives. If you’re concerned about yourself or someone you care about, know that you’re not alone and that help is available. A mental health professional can provide guidance, support, and the right treatment plan for your unique situation.
If you have questions or need support, The Haven Detox is here to help you on your journey toward wellness.
Get answers about your cost / coverage now.
Your information will be kept private
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
Need someone to talk to? We’re always here—day or night.
Ask questions, get guidance—no pressure, no obligation.
Your story stays with us. Confidential support, always.


Why Wait?
Get Answers Now
You’re here because you know you need help. Let’s talk through it together. There’s no commitment and it’s 100% confidential even to check your insurance.
100% Confidential


Why Wait?
Get Answers Now
You’re here because you know you need help. Let’s talk through it together. There’s no commitment and it’s 100% confidential even to check your insurance.
100% Confidential