Dr. Rostislav Ignatov, MD
Chief Medical Officer
If you’ve been researching naltrexone, you’ve probably noticed how mixed the information can feel. Some sources describe it as a powerful medication for alcohol or opioid use. Others make it sound ineffective, harsh, or confusing to start. That disconnect leaves many people unsure whether naltrexone is actually worth considering.
Naltrexone is a well-studied, FDA-approved medication used in the treatment of alcohol use disorder and opioid use disorder. But it’s also one of the most misunderstood medications in addiction care. It doesn’t stop withdrawal or replace medical detox. It doesn’t create a sense of calm or relief right away. And for some people, the effects are subtle rather than dramatic.
This page focuses on how naltrexone is used in real life. That includes what it does well, where it falls short, and why expectations matter so much when deciding if it’s the right fit. The goal is to help you understand what naltrexone can realistically offer, not to oversell it or dismiss it.
Table of Contents
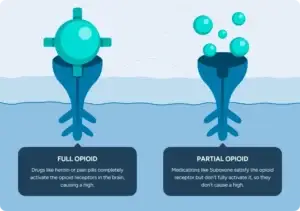
Naltrexone is approved to help treat alcohol use disorder (AUD) and opioid use disorder (OUD). It works differently from medications like buprenorphine or methadone and is not considered an opioid itself.
For alcohol use disorder, naltrexone is used to reduce the rewarding effects of drinking. Many people report that alcohol feels less satisfying over time, which can make it easier to drink less or avoid alcohol altogether.
For opioid use disorder, naltrexone blocks the effects of opioids at specific receptors in the brain. If opioids are used while naltrexone is active, they do not produce the usual euphoric effects. This makes relapse less reinforcing and can support long-term behavior change for some people.
One of the biggest sources of frustration with naltrexone comes from what it doesn’t do.
Naltrexone does not treat withdrawal symptoms or replace medical withdrawal management during detox. It does not ease nausea, anxiety, body aches, or insomnia during detox. It also does not help with pain and cannot be used while someone is actively taking opioids.
It’s also important to understand that naltrexone does not eliminate cravings overnight. For many people, changes are gradual. The medication works best when it’s paired with therapy, structure, and ongoing support rather than used on its own.
Understanding these limits early helps prevent disappointment and makes it easier to decide whether naltrexone fits into a broader treatment plan.
When naltrexone is started for the right reasons and at the right time, it can be a helpful tool. When it’s expected to do things it was never designed to do, people often stop it early or assume it “failed.”
Clear expectations are one of the strongest predictors of whether someone sticks with this medication long enough to see benefit.
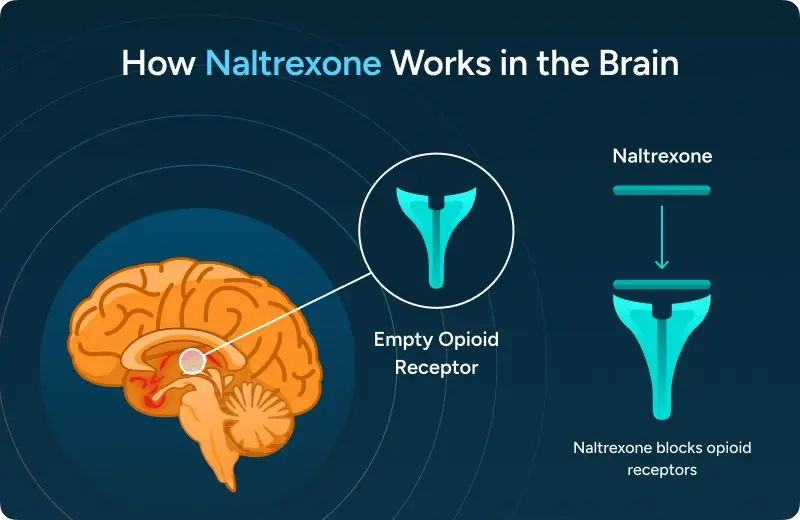
Naltrexone works by attaching to opioid receptors in the brain. These receptors are involved in how the brain experiences reward and reinforcement from substances like alcohol and opioids.
When naltrexone is active, it blocks those receptors. If alcohol or opioids are used, the usual rewarding effects are reduced or absent. There is no high, no sedation, and no calming effect created by the medication itself. Instead, the brain receives less reinforcement from the substance.
This is an important distinction. Naltrexone does not change mood or provide immediate relief the way some medications do. Its role is quieter. Over time, repeated use of a substance becomes less rewarding, which can make it easier to change behavior and reduce use.
One reason naltrexone is often misunderstood is because many people don’t “feel” it working right away.
Unlike medications that directly reduce anxiety or withdrawal symptoms, naltrexone works in the background. The brain may still recognize habits, routines, or stress triggers, even though the reward response is dampened. Because of that, early changes are often noticed in hindsight rather than immediately.
For example, someone may realize after a few weeks that urges feel less intense, drinking feels less appealing, or a lapse doesn’t spiral the way it used to. These shifts are gradual, which can be discouraging if someone expects fast or dramatic effects.
Not everyone responds to naltrexone in the same way. Differences in brain chemistry, substance use history, genetics, and environment all play a role.
Some people notice clear changes in how substances affect them. Others experience more modest benefits that only become meaningful when combined with therapy, structure, and accountability. This doesn’t mean the medication isn’t working. It means that naltrexone is one tool, not a standalone solution.
Understanding how it works helps explain why consistency and support matter so much when using this medication.
You may see naltrexone discussed in connection with other conditions or experimental uses. This usually reflects ongoing research or off-label prescribing in very specific situations, not standard treatment for substance use disorders.
These uses are not interchangeable with addiction treatment, and they require careful medical oversight. If something you’ve read online doesn’t seem to match your situation, that’s a sign to ask questions rather than assume it applies.
Cravings aren’t just thoughts about drinking or using. They’re a mix of physical urges, emotional responses, and learned habits. Stress, certain places, social cues, and even time of day can all trigger them.
Naltrexone doesn’t erase these triggers. Instead, it changes what happens after a substance is used. By blocking the brain’s reward response, the medication can reduce how reinforcing alcohol or opioids feel over time. For many people, that leads to cravings becoming less intense or less persistent, even if they don’t disappear completely.
Some people notice changes within the first week or two. Others need several weeks of consistent use before cravings start to shift. This timeline often depends on how long someone has been using substances, how strong their triggers are, and whether the medication is combined with therapy or structured support.
It’s common for people to stop naltrexone too early because they expect an immediate change. In reality, the benefit often builds gradually as the brain learns that alcohol or opioids no longer deliver the same reward.
If cravings feel unchanged at first, that doesn’t automatically mean naltrexone isn’t effective. Sometimes the medication is working, but the habits and emotional triggers around substance use are still very active.
In other cases, naltrexone may not be the best fit. Some people respond better to different medications or need additional support before the benefits become noticeable. Adjustments in dose, formulation, or treatment approach may also make a difference.
What matters most is not labeling the experience as a failure. Medication response is individual, and finding the right approach often takes time and guidance.
Contrave is a prescription medication that combines naltrexone with bupropion and is approved for weight management, not for treating alcohol or opioid use disorder. The doses and goals are different from how naltrexone is used in addiction treatment.
Because of this, information about Contrave can be confusing for people researching naltrexone. Using or combining medications without medical guidance can be unsafe, especially when substance use, withdrawal risk, or other mental health conditions are involved.
Naltrexone works best when it’s part of a broader plan. Therapy, counseling, and practical coping strategies help address the stress and patterns that medication alone can’t change.
When expectations are realistic and support is in place, naltrexone can make cravings easier to manage and reduce the pull toward repeated use. For many people, that shift creates enough space to focus on longer-term change.
Naltrexone can only be started safely once opioids are completely out of the body, which often requires opioid detox first. If it’s taken too soon, it can trigger precipitated withdrawal, which is a sudden and intense form of opioid withdrawal. This happens because naltrexone forcefully pushes opioids off their receptors.
For most people, this means waiting:
This waiting period can feel frustrating, but it’s critical. Starting naltrexone too early doesn’t just cause discomfort. It can derail treatment entirely and make people hesitant to try medication again.
Because timing matters, medical guidance is essential when deciding when to start.
Oral Naltrexone
(Daily Tablet)
Oral Naltrexone
(Daily Tablet)
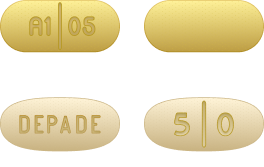
Naltrexone is available in two main forms:
Oral naltrexone allows more flexibility. It can be started and stopped quickly and may be preferred by people who want more control or are still deciding if the medication is right for them. The downside is consistency. Missing doses reduces effectiveness.
Injectable naltrexone provides steady coverage for a full month. It removes the need to remember daily medication and can be helpful for people who struggle with adherence. However, once given, it cannot be reversed, which makes proper screening and timing even more important.
The “better” option depends on medical history, lifestyle, and treatment goals.
Naltrexone is processed by the liver, so basic blood work is usually done before starting. This doesn’t mean the medication is unsafe. It means providers want to be sure the liver can handle it appropriately.
Mild to moderate liver enzyme elevations don’t always rule out naltrexone, but they do influence how closely someone is monitored. Heavy ongoing drinking can also increase liver strain, which is another reason medical oversight matters.
Starting naltrexone isn’t just about writing a prescription. It involves timing, lab work, symptom monitoring, and follow-up. Medical supervision helps reduce risks, manage side effects early, and adjust the plan if something doesn’t feel right.
When naltrexone is started thoughtfully and with support, people are far more likely to stay on it long enough to see benefit.
Unsure when it’s safe to start naltrexone?
Starting this medication too early can cause serious withdrawal. A medical detox team can help determine timing, safety, and next steps based on recent substance use.
The most commonly reported side effects with naltrexone include nausea, headache, fatigue, and mild dizziness. These symptoms tend to show up early, often within the first few days of starting the medication.
For many people, these effects are temporary. As the body adjusts, symptoms often ease within one to two weeks. Taking oral naltrexone with food, staying hydrated, and starting at a lower dose before increasing can sometimes help reduce discomfort.
It’s also worth noting that early side effects can overlap with stress, sleep disruption, or lingering effects from recent substance use. That overlap can make it hard to tell what’s causing what, which is another reason follow-up matters.
Topic
Use
Nausea and Appetite Changes
Fatigue and Headaches
Liver Health and Naltrexone
Nausea is one of the most common concerns people search for. It can range from mild queasiness to a stronger stomach upset, especially at the beginning.
This happens because opioid receptors also play a role in the digestive system. When those receptors are blocked, the gut can feel “off” until it adjusts. Appetite changes may occur alongside nausea, but significant weight loss is not a typical or expected effect at standard doses used for addiction treatment.
If nausea is persistent or severe, providers may adjust dosing or timing rather than stopping the medication outright.
Some people feel more tired than usual or develop headaches after starting naltrexone. These effects are usually mild but can feel discouraging if someone expects to feel better right away.
Fatigue doesn’t mean the medication is sedating the brain. Instead, it’s often related to changes in stress signaling, sleep patterns, or the body adjusting to blocked opioid receptors. Headaches tend to improve with time and basic measures like hydration and regular meals.
Because naltrexone is processed by the liver, concerns about liver damage are common. At standard therapeutic doses, serious liver injury is uncommon, but monitoring is still important.
Providers typically check liver enzymes before starting and may repeat labs during treatment, especially if someone has a history of liver disease or heavy alcohol use. Symptoms like yellowing of the skin or eyes, dark urine, or persistent abdominal pain should always be reported right away.
This monitoring is precautionary and meant to keep treatment safe, not to exclude people unnecessarily.
Topic
Nausea and Appetite Changes
Description
Nausea is one of the most common concerns people search for. It can range from mild queasiness to a stronger stomach upset, especially at the beginning.
This happens because opioid receptors also play a role in the digestive system. When those receptors are blocked, the gut can feel “off” until it adjusts. Appetite changes may occur alongside nausea, but significant weight loss is not a typical or expected effect at standard doses used for addiction treatment.
If nausea is persistent or severe, providers may adjust dosing or timing rather than stopping the medication outright.
Topic
Fatigue and Headaches
Description
Some people feel more tired than usual or develop headaches after starting naltrexone. These effects are usually mild but can feel discouraging if someone expects to feel better right away.
Fatigue doesn’t mean the medication is sedating the brain. Instead, it’s often related to changes in stress signaling, sleep patterns, or the body adjusting to blocked opioid receptors. Headaches tend to improve with time and basic measures like hydration and regular meals.
Topic
Liver Health and Naltrexone
Description
Because naltrexone is processed by the liver, concerns about liver damage are common. At standard therapeutic doses, serious liver injury is uncommon, but monitoring is still important.
Providers typically check liver enzymes before starting and may repeat labs during treatment, especially if someone has a history of liver disease or heavy alcohol use. Symptoms like yellowing of the skin or eyes, dark urine, or persistent abdominal pain should always be reported right away.
This monitoring is precautionary and meant to keep treatment safe, not to exclude people unnecessarily.
Most side effects are mild and short-lived, but some situations need medical input. Ongoing vomiting, severe abdominal pain, confusion, or symptoms that worsen instead of improve should be discussed promptly.
Stopping naltrexone suddenly without guidance isn’t ideal either. A provider can help determine whether symptoms are related to the medication, another health issue, or something that can be managed with simple adjustments.
Naltrexone is not a weight loss medication when used on its own at standard doses. Some people notice small changes in appetite early on, often related to nausea or reduced interest in alcohol, but meaningful or consistent weight loss is not a reliable effect.
Weight loss discussions usually come from a different context, involving combinations or lower doses used for other conditions. For alcohol or opioid use disorder, naltrexone is prescribed to reduce the rewarding effects of substances, not to manage weight.
Some people do drink alcohol while taking naltrexone. Physically, the medication does not cause a dangerous reaction with alcohol the way some other medications do. However, that does not mean drinking is risk-free.
Naltrexone reduces the rewarding effects of alcohol. For many people, drinking feels less satisfying, and the urge to keep drinking fades sooner. At the same time, alcohol can still impair judgment, coordination, and reaction time. Because of that, someone may drink more than intended while trying to “feel” the effects, which increases the risk of poor decisions or liver strain.
Naltrexone is meant to support reduced drinking or abstinence, not to make heavy drinking safer.
Using opioids while naltrexone is active is far more dangerous.
Naltrexone blocks opioid receptors. If opioids are used, the usual effects are reduced or absent. Some people interpret this as protection, but it is not. Trying to override the blockade by taking more opioids can lead to respiratory depression, overdose, or death, especially if the medication wears off or doses are missed.
Another major risk happens if naltrexone is stopped. Opioid tolerance drops while the medication is in the system. A dose that once felt manageable can become life-threatening after even a short break from opioids.
A slip does not mean treatment has failed. It does mean safety needs to be addressed right away.
The most important step after any alcohol or opioid use while on naltrexone is to talk to a medical provider. Adjustments, added support, or a different treatment approach may be needed. Shame and secrecy increase risk. Honest conversations reduce it.
Naltrexone is one tool. Its purpose is to reduce risk and support change, not to punish setbacks.
If someone has used opioids while on naltrexone, has severe breathing problems, collapses, or cannot be awakened, emergency care is critical.
If there is uncertainty about what was taken or how much, it’s always safer to call 911 immediately. Acting quickly can save a life.
Concerned about recent alcohol or opioid use?
Using substances while on naltrexone can increase risk. If you’re unsure what to do next, medical guidance can help prevent complications and keep things from getting worse.
Because naltrexone is processed by the liver, people with active or severe liver disease may need extra caution. Mild to moderate liver enzyme elevations do not automatically rule it out, but they do affect how closely someone should be monitored.
This is why blood work is checked before starting and sometimes repeated during treatment. The goal is safety, not gatekeeping. In many cases, providers can still use naltrexone with careful follow-up, especially if the potential benefits outweigh the risks.
Naltrexone blocks opioid receptors, which means opioid pain medications will not work while it’s active. This can be a serious issue for people who:
Pregnancy, breastfeeding, and certain mental health or medical conditions require individualized decision-making. Research on naltrexone in pregnancy is limited, so providers weigh potential risks and benefits carefully rather than applying a one-size-fits-all rule.
Other factors like past medication response, co-occurring mental health conditions, and treatment goals also influence whether naltrexone is a good fit. What works well for one person may not be the right choice for another.
Naltrexone can reduce the reinforcing effects of alcohol or opioids, but it doesn’t change the stressors, habits, or emotional patterns that often drive substance use. This is why it’s typically used as part of medication-assisted treatment, alongside therapy and structured support. That’s why outcomes tend to be better when medication is paired with therapy, structure, and practical coping strategies.
Counseling and behavioral therapies help people recognize triggers, manage stress, and respond differently when urges show up. Support also creates accountability and problem-solving when progress feels slow or uneven. Together, these pieces make the benefits of naltrexone more noticeable and more sustainable.
The most effective treatment plans are flexible. Needs change over time, and medication plans sometimes do too. Some people stay on naltrexone for months, others longer, and some transition to different supports as goals evolve. What matters most is that the plan fits real life and adjusts when something isn’t working. That adaptability is often what makes long-term improvement possible.
If you’re looking into naltrexone, it’s usually because you want things to feel more manageable or safer as soon as possible. For many people, that starts with understanding whether medication can be used right away or whether detox is the safest place to begin.
Naltrexone can be helpful, but it isn’t started the same way for everyone. Recent alcohol or opioid use, withdrawal risk, and medical history all matter. A medical evaluation can help clarify what’s possible now and what needs to happen first.
Thinking about naltrexone? It often starts with detox.
A medical team can help explain options, timing, and safety so the next step makes sense for your situation.
Get answers about your cost / coverage now.
Your information will be kept private
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!