Aetna Insurance Coverage for Detox, Addiction & Mental Health Treatment
If you’re worried about starting detox and addiction treatment, that’s common. Even with insurance, the costs can feel like one more obstacle to getting help and feeling better. This guide shows you what different Aetna plans cover and what you need to get coverage approved.
Aetna offers several plans to help with the cost of addiction treatment. Its PPOs, including Open Choice and Managed Choice, cover inpatient and outpatient treatment, including IOPs and PHPs. Aetna typically covers detox treatment, therapy, medication, and other types of mental health treatment to support your wellness long-term.
With other plan options, including HMOs, EPOs, HDHPs, and Medicare plans, you can get more affordable, accessible care. The specific coverage depends on your plan. Always check your benefits before you start treatment.
Level of Care
Typically Covered?
Prior Authorization
Typical Length
Medical Detox
Inpatient / Residential
Partial Hospitalization (PHP)
Intensive Outpatient (IOP)
Outpatient Therapy
Sometimes
5–14 days
14–28+ days
4–8 weeks
8–12 weeks
Ongoing
Level of Care
Medical Detox
Typically Covered?
Yes
Prior Authorization
Required
Typical Length
5–14 days
Level of Care
Inpatient / Residential
Typically Covered?
Yes
Prior Authorization
Required
Typical Length
14–28+ days
Level of Care
Partial Hospitalization (PHP)
Typically Covered?
Yes
Prior Authorization
Required
Typical Length
4–8 weeks
Level of Care
Intensive Outpatient (IOP)
Typically Covered?
Yes
Prior Authorization
Required
Typical Length
8–12 weeks
Level of Care
Outpatient Therapy
Typically Covered?
Yes
Prior Authorization
Sometimes
Typical Length
Ongoing
Service Type
Covered by Aetna
What’s Included
Prior Authorization
Psychiatric Evaluation
Inpatient Psychiatric Care
Residential Mental Health Treatment
Partial Hospitalization (PHP)
Intensive Outpatient Program (IOP)
Outpatient Therapy
Psychiatric Medication
Telehealth Services
Diagnostic assessment, medication review, treatment planning
24/7 supervision, crisis stabilization, medication management
Structured daily therapy, psychiatric oversight, ongoing evaluation
4–6 hours of treatment per day, 5–7 days per week
2–3 hours per session, 3–5 days per week
Individual, group, family, and multi-family therapy
Covered based on formulary tier
Therapy and psychiatry via secure video
Sometimes
Sometimes
Sometimes
Sometimes
Service Type
Psychiatric Evaluation
Covered by Aetna
Yes
What’s Included
Diagnostic assessment, medication review, treatment planning
Prior Authorization
Sometimes
Service Type
Inpatient Psychiatric Care
Covered by Aetna
Yes
What’s Included
24/7 supervision, crisis stabilization, medication management
Prior Authorization
Required
Service Type
Residential Mental Health Treatment
Covered by Aetna
Yes
What’s Included
Structured daily therapy, psychiatric oversight, ongoing evaluation
Prior Authorization
Required
Service Type
Partial Hospitalization (PHP)
Covered by Aetna
Yes
What’s Included
4–6 hours of treatment per day, 5–7 days per week
Prior Authorization
Required
Service Type
Intensive Outpatient Program (IOP)
Covered by Aetna
Yes
What’s Included
2–3 hours per session, 3–5 days per week
Prior Authorization
Required
Service Type
Outpatient Therapy
Covered by Aetna
Yes
What’s Included
Individual, group, family, and multi-family therapy
Prior Authorization
Sometimes
Service Type
Psychiatric Medication
Covered by Aetna
Yes
What’s Included
Covered based on formulary tier
Prior Authorization
Sometimes
Level of Care
Telehealth Services
Covered by Aetna
Yes
What’s Included
Therapy and psychiatry via secure video
Prior Authorization
Sometimes



1
Aetna covers evidence-based, 24/7 detox services for withdrawal from alcohol, benzodiazepines, and opioids. That includes nursing treatment and physician care at Aetna detox centers, as well as medications during detox.
There’s no set amount of time Aetna approves. Usually, it starts with 7 days of approved coverage for detox. But detox often takes longer than that. Aetna may extend your coverage depending on what substances you’ve used and the risks you’d face without medical detox.
To approve longer coverage, Aetna needs updates from your provider. You may need to call Aetna before your approval period ends to get it extended.
Detox is typically a short-term part of your treatment. Aetna will approve it until it’s safe for you to transition to other types of care, like inpatient rehab or an IOP.
2
Aetna covers psychiatric hospitalization focused on evaluating and stabilizing your condition. It includes psychiatric evaluation, crisis stabilization, medication management, and detox.
Aetna covers evidence-based forms of therapy, including cognitive behavior therapy (CBT), dialectical behavior therapy (DBT), eye movement desensitization and reprocessing (EMDR), and mindfulness-based cognitive therapy (MBCT). It generally covers individual, group, and family therapy sessions.
Aetna uses the Level of Care Utilization System (LOCUS) to approve your care.2 This system helps Aetna decide what type of care you need, but it’s not the only factor that affects approval. LOCUS has 6 levels of care, with 0 and 1 requiring the least intense care and 6 needing the most intensive care. These levels include:
Aetna inpatient rehab doesn’t have a specific approval length. Initially, it will take 7 to 14 days for substance use-related psychiatric hospitalization. For psychiatric hospitalization without substance use, Aetna may approve 5 to 10 days at first.
Your treatment center will need to update Aetna while you’re in their care. Based on these updates, Aetna will approve a longer stay. Often, it takes 6 to 8 weeks, but it may take up to 90 days. The approval depends on medical necessity and the reports your treatment center sends.
3
Aetna approves 24/7 rehab treatment for substance use disorder and co-occurring mental health conditions. Your coverage includes your stay at the residential treatment center, medication management, and evidence-based therapies for individuals, groups, and families. The goal of Aetna’s residential mental health treatment is to assess your condition and stabilize you.
Aetna also considers factors from the American Society for Addiction Medicine (ASAM) for substance use treatment cases. These criteria help determine what level of care for addiction treatment is best for you. ASAM criteria include:
Level of Care
Support Level
Who It’s For
Aetna Coverage
Inpatient Psychiatric
Residential Treatment
Partial Hospitalization (PHP)
Intensive Outpatient (IOP)
Outpatient Therapy
Immediate safety concerns
Ongoing instability
Needs daily structure
Needs frequent support
Stable symptoms
Level of Care
Inpatient Psychiatric
Support Level
Highest
Who It’s For
Immediate safety concerns
Aetna Coverage
Covered
Level of Care
Residential Treatment
Support Level
Very High
Who It’s For
Ongoing instability
Aetna Coverage
Covered
Level of Care
Partial Hospitalization (PHP)
Support Level
Moderate–High
Who It’s For
Needs daily structure
Aetna Coverage
Covered
Level of Care
Intensive Outpatient (IOP)
Support Level
Moderate
Who It’s For
Needs frequent support
Aetna Coverage
Covered
Level of Care
Outpatient Therapy
Support Level
Low
Who It’s For
Stable symptoms
Aetna Coverage
Covered
Aetna approves your treatment based on medical necessity, not a set length of time. It initially approves treatment based on a 28-day model.1 After that, Aetna will reassess your treatment plan and extend your stay if needed. To approve these extensions, Aetna needs periodic updates on your treatment progress.
4
Aetna covers a partial hospitalization program for substance use disorder and other mental health conditions. It’s often meant to help you transition from residential to outpatient treatment.
An Aetna partial hospitalization program includes medical support from physicians, nurses, and mental health clinicians. These programs take place 5 to 7 days a week at a treatment center. You receive treatment for 4 to 6 hours each day you’re there. That treatment includes individual, group, family, and multi-family therapy. It also helps with medication management.
Your Aetna PHP coverage length depends on what you need for your treatment process. Most of the time, PHPs last 4 to 8 weeks. Some programs are only 2 to 4 weeks, so you’ll likely get a shorter time approved first. Aetna needs regular updates about your treatment to decide whether they’ll extend it.
5
Aetna covers intensive outpatient programs as another step from residential to outpatient treatment. Most IOPs offer treatment 3 to 7 days a week for 2 to 3 hours a day. While you get treatment, you stay at home and can still do your daily activities, like going to work or school. You don’t stay overnight at the facility.
Aetna covers individual, group, family, and multi-family therapy as part of your IOP. The programs also offer educational services to help you cope outside of the program. Your plan may even cover a virtual IOP.
Aetna doesn’t approve a set time for IOPs. Most IOPs last 8 to 12 weeks. Aetna IOP coverage will likely be approved for 2 to 4 weeks initially, but you can often extend it to 6 to 12 weeks.
Your approval extension depends on updates from your treatment center. Aetna will review these updates and extend your program coverage if standard outpatient care does not offer enough support.
6
Aetna outpatient mental health benefits cover evidence-based therapies with a licensed therapist or psychiatrist. That can include:
Aetna will typically approve individual, group, family, and multi-family therapy. That includes counseling, medication management, and psychiatric evaluations. You can often get telehealth sessions approved, too.
Outpatient therapy can be short-term or last for years. It depends on your mental health and therapy needs. Even after you’re out of crisis and are maintaining your wellness, therapy can help you deal with stress and setbacks before they get serious.
Aetna typically approves 12 to 20 visits per year. You may have a limit on the number of visits with your plan. However, some states prohibit these limits. Aetna will review regular reports from your therapist or psychiatrist to extend your coverage.
Aetna covers medication-assisted treatment (MAT) with FDA-approved medications. Those may include:
It approves MAT when combined with therapy. You may need to get pre-authorization from Aetna before you receive MAT. This is more common with Medicare and Medicaid plans than with Aetna’s traditional plans. Aetna looks at whether you have been diagnosed with substance use disorder with substances like opioids, benzodiazepines, or alcohol.
7
Aetna doesn’t usually cover sober living. Sober living situations aren’t considered medical facilities. Their regulations vary too much for most insurance to cover.
Sober living can offer support for you if you’ve been through treatment and need more help to stay well. However, you’ll most likely need to pay for them out-of-pocket.
You want to feel prepared before you go through addiction treatment. It can make the process feel less scary and help you decide your next steps. Knowing what you need to pay out of pocket and what insurance will cover can help you focus on getting and staying well.
Aetna covers many services, but it may not pay 100% of your treatment costs. Most of the time, you need to reach your deductible first. Aetna deductibles range from $1,700 to $5,000. The amount depends on whether you have an individual or family plan, your plan type, and your plan network.
After the deductible, you’ll have to pay coinsurance. With coinsurance, Aetna covers a certain percentage of your care, and you pay the rest until you hit your out-of-pocket maximum. For in-network care, you’ll typically pay 10 to 30% out-of-pocket. For out-of-network care, you may need to cover up to 50% of the cost.
Once you hit your out-of-pocket maximum, Aetna will cover your full treatment cost.
Aetna offers much more coverage for in-network providers. But it still covers out-of-network treatment centers with many of its plans. You’re more likely to get out-of-network coverage if you have a PPO. HMO plans usually don’t cover any out-of-network services, except for emergency care.
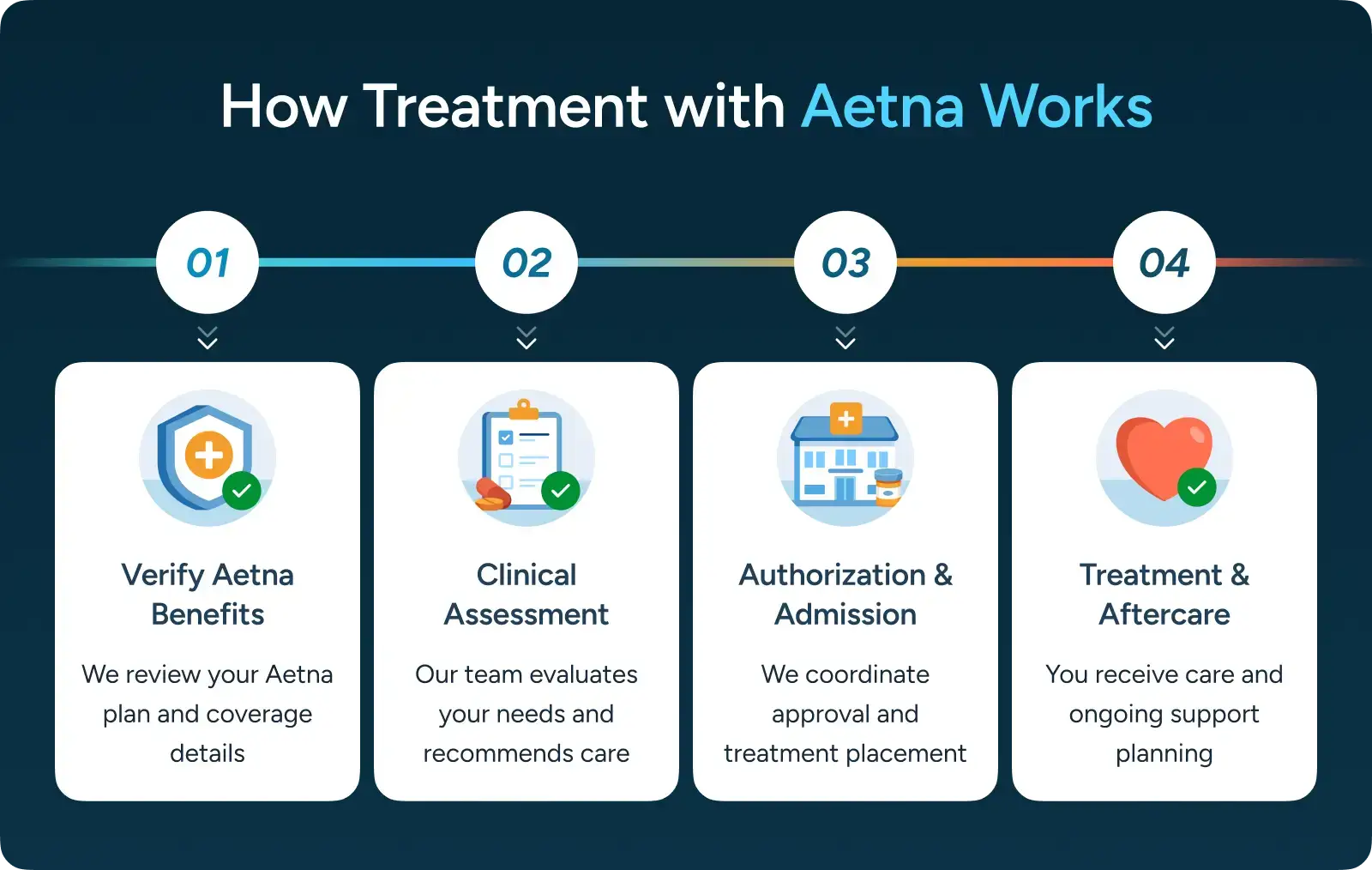
Your treatment center works with Aetna to help you get covered treatment for substance use. The treatment center will verify your coverage before you start care. They can explain your costs and get a pre-authorization if you need one.
You can also use Aetna’s online provider search tool as a member or a guest to find treatment centers near you.
Accepts Aetna

Accepts Aetna

Aetna Employer Plans in Florida
Aetna only offers employer group plans in Florida. These plans include its traditional Open Choice and Managed Choice PPOs, Health Network Only HMO, Premier Care Network, and all other current Aetna plan offerings.
Aetna Commercial Plans in Florida
As of December 2025, Aetna has stopped offering commercial plans on the ACA Marketplace in Florida. Aetna has also done away with its CVS Health plan. Aetna has help available for you to transition to another insurance plan.
Aetna & Florida Medicaid
Aetna Better Health works with Florida Medicaid to give qualifying residents access to healthcare. Aetna offers Medicaid options to three Florida regions with its Managed Medical Assistance and Long-Term Care plans.
Florida Unique Aetna Coverage Information
Florida offers some protections for you to get emergency care if you need it. The Marchman Act, which deals with substance use cases, and the Baker Act, for psychiatric care, give you access to emergency stabilization without pre-authorization. You’ll still need prior authorization before you can continue with inpatient or outpatient care after you’re stable.
Accepts Aetna

Aetna Employer Plans in Massachusetts
Aetna only offers employer plans in Massachusetts as of January 2026. This includes its most popular traditional PPO plans, as well as its HMO, EPO, and HDHP options.
Aetna Commercial Plans in Massachusetts
Aetna no longer offers plans through the Massachusetts ACA Marketplace. It removed its plans due to financial losses and company costs. You can find other insurance options through the Massachusetts HealthConnector.
Aetna & Massachusetts Medicaid
Aetna’s Medicaid Managed Care Organizations are available in many states, including Massachusetts. Aetna also works with MassHealth, the Massachusetts Medicaid program, to cover your medical costs. If you have an Aetna Medicaid plan, Aetna will pay a portion of your care first. Then, MassHealth will cover the rest of the eligible amount.
Massachusetts Unique Aetna Coverage Information
Massachusetts is one of the leading states for mental health coverage. The state’s Mental Health Parity Law requires practices and insurance to treat mental health with the same level of importance as physical health. It also prevents insurers from imposing stricter limits on substance use treatment than on other types of mental health treatment.
The Mental Health ABC Law, passed in 2022, has removed prior authorization requirements for acute mental healthcare. It also guarantees you the opportunity for an annual mental wellness exam. Massachusetts legally must cover your mental health treatment for several conditions, including major depression, PTSD, and bipolar disorder.
Accepts Aetna

Aetna Employer Plans in New Jersey
All Aetna plans in New Jersey are employer plans. Aetna offers many plans throughout New Jersey, including the Garden State Health Plan. This plan uses the Aetna Whole Health network for state and school employees. Aetna also offers several plans with a health savings account, such as the tiered Freedom plan and the Freedom HDHigh/HDLow plan, Aetna HMO, and Aetna Liberty Plus plans.
Aetna Commercial Plans in New Jersey
Aetna no longer offers commercial plans on the ACA Marketplace anywhere in the country. The company stated it was leaving the marketplace in 2026 due to company costs and financial losses.
Aetna & New Jersey Medicaid
Aetna offers its Better Health Medicaid plans through NJ FamilyCare. These plans are available in every county in the state. In New Jersey, you only pay copays for your care. When Aetna pays providers, the provider accepts that as full payment if you have Medicaid. The provider can’t bill you for additional charges on a covered service. For non-covered services, you may be able to get written notice and sign an agreement for Aetna to pay your costs.
New Jersey Unique Aetna Coverage Information
New Jersey is known for high-quality mental healthcare, including for substance use treatment. The state’s Mental Health Parity Act requires that mental health be treated as seriously as physical health.
New Jersey has worked to lower barriers to mental healthcare. It has shorter wait times than many nearby states. Plus, it works to reduce pre-authorization requirements, so you can get care faster.
Accepts Aetna


Aetna Employer Plans in Arkansas
Aetna only offers employer group plans in Arkansas. As of January 2026, Aetna has stopped offering its Aetna CVS Health plan, which was an individual plan you could get through Arkansas’s ACA Marketplace.
Aetna Exchange Plans in Arkansas
Aetna no longer offers individual plans on the Arkansas Health Insurance Marketplace. It only offers plans through employers.
Aetna & Arkansas Medicaid
Aetna offers Medicare Advantage plans in Arkansas, including PPOs like Medicare Value Plus and Medicare Eagle Giveback. Aetna does not work with ARHOME to provide health insurance coverage.
Arkansas Unique Aetna Coverage Information
Some of Arkansas’s Medicaid plans have fewer restrictions and requirements than traditional plans, like Aetna PPOs. You may not need a pre-authorization with these plans if you’re looking for MAT treatment. Most Aetna plans still require you to get a pre-authorization.
Accepts Aetna


You have a few options to verify your Aetna behavioral health benefits. You can log into the Aetna member website or use the Aetna Health app to check your coverage. Or, check the back of your insurance card to find the most accurate phone number to call about your benefits. Aetna’s general employer and group coverage number is 1-800-307-4830.
If you need to find out if you’re covered at a specific treatment center, you can call that facility. They can tell you which plans they accept, explain what your plan covers, and tell you the expected cost to you. The treatment center can also tell you if you need prior authorization and submit that for you.

Pre-authorization works differently from a referral. Aetna needs to review your medical reports to decide whether your treatment is safe and likely to support your care needs. The pre-authorization means Aetna has approved you for coverage before you start care.
Aetna requires you to get pre-authorization before most inpatient and outpatient mental health services. The exception is for emergency stabilization care. After the emergency period, you will need pre-authorization for most residential, PHP, IOP, and outpatient programs. Some plans also require it for medication approval.
If you need prior authorization, your treatment center will submit it for you.
You’ll get a denial letter in the mail if Aetna doesn’t approve your coverage. If this happens, you can submit an appeal.
For most policies, you need to request an appeal within 60 days of Aetna’s initial decision. You can file your appeal on Aetna’s website or fill out the appeal forms. If you have a serious health situation, you can request an urgent appeal. If not, you can ask for a peer-to-peer review where your healthcare provider reviews your case with Aetna.
If you get denied again, you can request an external appeal to make a final decision.
Yes, if you meet Aetna’s criteria for medical necessity. Aetna approves your coverage if you have a high risk of severe withdrawal symptoms like delirium tremens, seizures, or dangerous changes to your vital signs.
Typically, medical detox for opioids, benzodiazepines, and alcohol is covered. You may also get coverage for other types of substance use, but it depends on the severity of your condition.
Most detox programs last 5 to 14 days. Aetna may approve a shorter stay initially, but this can be extended.
Aetna covers psychiatric medications for mental health conditions, including anxiety, depression, PTSD, bipolar disorder, ADHD, and more. These medications are often covered along with therapy.
You may need to get pre-authorization from Aetna before you get coverage approved. Medication copays vary, but with Aetna’s Tier 1 medications, you may pay less than $20 per prescription.
Aetna covers eating disorder treatment when you have a diagnosis of an eating disorder and meet Aetna’s guidelines for needing care. It covers eating disorder assessments, including blood tests, bone density measurements, liver function tests, psychiatric evaluations, and more. You can also get nutrition counseling, medication management, therapy, and treatment at the PHP, IOP, and outpatient levels.
Aetna therapy coverage includes individual, group, family, and multi-family sessions. It only covers evidence-based therapies, including CBT, DBT, EMDR, and MBCT. This includes telehealth sessions.
There’s no set number of therapy sessions Aetna approves. Some states, like Massachusetts, have a minimum number required for approval. Many states legally prevent insurance from limiting the maximum number of sessions you can receive.
Aetna needs periodic reports to continue to approve sessions yearly. You may also need a referral if you have certain types of Aetna plans, like an HMO. With PPOs, you don’t usually need a referral.
Aetna covers family therapy and multi-family therapy if it’s necessary for your treatment process. The same applies to couples counseling. Outside of a medical need for substance use or other mental health treatment, Aetna probably won’t cover it.
Check the coverage benefits of your specific plan before going to family or couples therapy. You may need a referral, though many Aetna plans don’t require one for therapy.
Aetna offers Medicare Advantage (Part C), Medicare Advantage with prescription drug coverage (MAPD), Stand-alone prescription drug plans (a Part D PDP), and Medicare Supplement Insurance Plans (Medigap).
The latter two plans are for people who have Original Medicare and help pay additional costs, like copays and deductibles. Your coverage may not be the same as you would have with a non-Medicare Aetna plan, so check your benefits for starting treatment.
You can always get emergency mental health care with Aetna. It doesn’t require a pre-authorization or a referral.
You can get care at the ER, psychiatric crisis units, and inpatient services for emergency care. Aetna lists crisis hotlines on its website. You can call 988 for confidential mental health crisis support, use the Lifeline Chat, or call the helpline for substance use services at 1-800-662-4357.
If you can’t pay out of pocket, you have several options:

Need someone to talk to? We’re always here—day or night.
Ask questions, get guidance—no pressure, no obligation.
Your story stays with us. Confidential support, always.
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!