
Dr. Rostislav Ignatov, MD
Chief Medical Officer
America’s substance use epidemic is evolving—but the nation’s help-seeking behavior isn’t keeping up.
A new study from The Haven Detox uses exclusive internal data along with national drug use data to reveal that hallucinogens, alcohol, and cannabis—some of the most widely used substances in the U.S.—are also among those least likely to drive people to seek help.
The study analyzes 2022–2023 data from the National Survey on Drug Use and Health and Haven’s own treatment records to provide previously unseen data on which substances have the greatest disparity between use and treatment.
Rather than access to care, this data reflects how cultural perception and substance effects influence help-seeking behavior. Substances like opioids are more likely to trigger intervention because of overdose risk and withdrawal. But substances like hallucinogens—while increasingly used—often don’t prompt users to seek treatment, even when harmful effects occur.
“The data doesn’t just show who’s using what—it shows who thinks they need help. That’s a different story entirely,” says Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management. – Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management
While substances like hallucinogens, alcohol, and cannabis often don’t prompt people to seek treatment, professional help is available regardless of which substance you’re struggling with. Our addiction treatment programs provide medically supervised detox and inpatient rehabilitation for all substance use disorders. For those with co-occurring mental health conditions, we offer integrated dual diagnosis treatment. Treatment is available in Arizona, Arkansas, Florida, Massachusetts, New Jersey, and Puerto Rico. Check your insurance coverage or review our insurance information. Contact our admissions team to begin treatment, regardless of which substance has become problematic.
Hallucinogens like psilocybin, LSD, and DMT now show the widest gap between use and help-seeking behavior. The data reveals 7.4 million annual users and only 320,000 treatment cases—a 1:23 ratio, in other words, 1 user seeking treatment for every 23 people using hallucinogens, the highest of any substance in the study.
Unlike opioids or alcohol, hallucinogens don’t cause physical dependency or withdrawal. Yet because these substances are often perceived as “mind-expanding” or “spiritually enlightening,” very few view their experiences as needing professional support.
“Hallucinogens are culturally framed as tools for healing and exploration. That framing may be silencing the need for help when things go wrong” – Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management
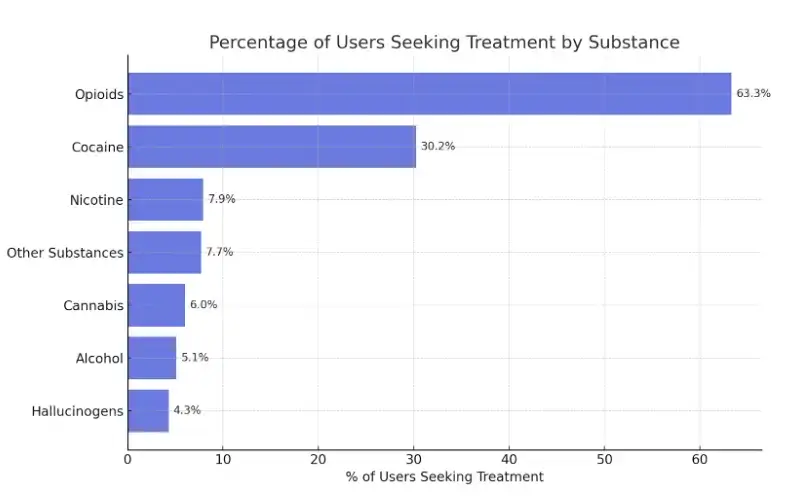
Opioids are one of the only substances in the study where treatment-seeking behavior keeps pace with use. With 5.1 million annual users and 3.2 million receiving treatment, the roughly 2:1 ratio indicates a far narrower disconnect compared to all other drugs analyzed. The existence of widespread, structured treatment programs—such as those involving methadone, buprenorphine, and naloxone—makes treatment more accessible and normalized.
Alcohol remains the most consumed substance in the country—with nearly 140 million past-month users. Yet only 7.1 million people sought treatment, yielding a 1:19 use-to-treatment ratio. That makes it the second most untreated substance by volume.
Because alcohol is embedded in American culture—from celebrations to stress relief—it can take years of misuse before someone considers seeking help.
Cannabis use has skyrocketed alongside legalization and shifting public opinion. According to the study, 61.9 million Americans used cannabis in the past year, but only 3.7 million received treatment, creating a 1:16 treatment ratio.
High frequency cannabis use has been linked to increased risk of anxiety, depression, motivation, and cognitive impairment.
“As cannabis use becomes more accepted, people are slower to admit when it starts negatively affecting their work, relationships, or mental health” – Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management
Cocaine, nicotine, and other illicit drugs fall into a middle tier—used widely enough to pose concern, but not often enough to drive consistent help-seeking behavior. Cocaine had 5.7 million users and 1.7 million treatment cases, yielding a 1:3 treatment ratio. While lower than alcohol or cannabis, the data suggests that many users delay seeking help until use escalates or becomes publicly visible.
Nicotine and other illicit substances show similar patterns. With 47.4 million nicotine users and 3.8 million in treatment, the 1:13 treatment ratio reflects a longstanding cultural normalization—particularly with the rise of vaping. Other illicit drugs, including meth and synthetic substances, have roughly a 1:13 ratio, shaped by regional stigma and inconsistent treatment access.
Cocaine, nicotine, and other illicit drugs fall into a middle tier—used widely enough to pose concern, but not often enough to drive consistent help-seeking behavior. Cocaine had 5.7 million users and 1.7 million treatment cases, yielding a 1:3 treatment ratio. While lower than alcohol or cannabis, the data suggests that many users delay seeking help until use escalates or becomes publicly visible.
Nicotine and other illicit substances show similar patterns. With 47.4 million nicotine users and 3.8 million in treatment, the 1:13 treatment ratio reflects a longstanding cultural normalization—particularly with the rise of vaping. In fact, young adults (ages 21–24) now account for the most prevalent vaping rates according to drug statistics, with 15.5% in 2023, highlighting how nicotine use has shifted toward younger generations. Other illicit drugs, including meth and synthetic substances, have roughly a 1:13 ratio, shaped by regional stigma and inconsistent treatment access.
“These aren’t the most ignored substances—but they’re often treated too late. People recognize the risks, but wait for things to get worse before acting” – Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management
America’s most-used substances—hallucinogens, alcohol, and cannabis—are also the ones people are least likely to seek treatment for, revealing a widening gap between use and help-seeking behavior.
States like Florida (1.28M), California (1.08M), and Texas (765K) report the highest total hallucinogen use, aligning with national increases in psychedelic experimentation. Per capita, Vermont (112.3), Alaska (63.7), and Colorado (69.2) lead the way—likely influenced by cultural openness and decriminalization efforts in those states.
Total Consumption (Thousands):
Per Capita (Users Per 1,000 Population):
In terms of raw volume, California (5.78M), Florida (2.99M), and New York (2.98M) lead the nation in alcohol consumption, unsurprising given their large populations. But on a per capita basis, Vermont (241.6), North Dakota (232.6), and Montana (210.9) show the highest concentration of drinkers, suggesting that alcohol use is deeply embedded in the culture of rural and smaller-population states.
Total Consumption (Thousands):
Per Capita (Users per 1,000 Population):
California (7.4M) and Florida (3.97M) top the list in total cannabis users. Yet Vermont (315.4), Maine (295.2), and Alaska (232.5) lead in per capita use, indicating more frequent or normalized cannabis consumption relative to population—particularly in states where legal access is well established.
Total Consumption (Thousands):
Per Capita (Users per 1,000 Population):
New York (917K), Florida (878K), and California (848K) account for the highest total cocaine use, reflecting patterns common in densely populated urban areas. However, per capita rankings shift the focus: Vermont (86.2), DC (74.4), and Massachusetts (50.4) have the highest user density, revealing surprising hotspots of use in smaller northeastern states.
Total Consumption (Thousands):
Per Capita (Users per 1,000 Population):
California (1.33M) had the most opioid misuse by volume, followed by Florida (786K) and Texas (683K). But the crisis is most concentrated in West Virginia (156.9), Kentucky (94.3), and Oklahoma (88.7) per 1,000 residents, highlighting the ongoing grip of opioids in Appalachia and rural America—where overdoses and economic hardship often intersect.
Total Consumption (Thousands):
Per Capita (Users per 1,000 Population):
This study suggests that help-seeking behavior is shaped less by how much people use a substance—and more by how dangerous, stigmatized, or physically addictive it is perceived to be.
In other words, what we fear most gets treated first. Substances like hallucinogens, despite growing popularity, don’t trigger the same urgency—even when users experience psychological distress, flashbacks, or emotional instability.
Critics might point out that hallucinogens don’t kill at the same rate as opioids or alcohol, and that they’re not physically addictive. Both are true. But that doesn’t mean they’re risk-free.
Unpredictable reactions, long-term dissociation, and psychotic episodes—especially among high-risk individuals—remain real outcomes for those using hallucinogens. The near-total lack of treatment-seeking for these issues represents a blind spot in current public health strategy – Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management
To close this disconnect, substance use care must evolve from a reactive, crisis-oriented model to a more proactive, perception-aware system. That includes:
“Hallucinogens, cannabis, and alcohol don’t cause the same public panic as opioids—but that’s exactly why they’re overlooked. We mistake silence for safety. The challenge now is to build a system that doesn’t just respond to what’s lethal, but to what’s quietly derailing lives in the background” – Dr. Rostislav Ignatov MD, Chief Medical Officer at Haven Health Management
This study utilizes data from the “2022-2023 National Survey on Drug Use and Health (NSDUH)” dataset and The Haven Detox data for treatment numbers.
State-level and total U.S. estimates were extracted for substance use from selected NSDUH tables, while substance use treatment data was sourced from The Haven Detox data.
Data analysis included compiling substance use data by state, calculating ratios of consumption to treatment at the national level, and identifying the top 5 states by both total and per capita consumption for each substance, with per capita rates calculated using state-level consumption estimates divided by state population.
Limitations of this study include reliance on NSDUH self-reported data, incomplete state-level data for all substances, use of both “past month” and “past year” consumption metrics, and the use of total state population for per capita calculations.
Get answers about your cost / coverage now.
Your information will be kept private
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!