Phoenix Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
Phoenix is experiencing significant disparities in treating addiction across neighborhoods, but the city has built a strong network of behavioral health services to support the community. Arizona recorded 2,539 drug overdose deaths in 2024, reflecting an 8.7% decline from 2023. Youth mental health trends are worsening: 2022 data show 17.3% of Arizona youth seriously considered suicide, and 8.6% attempted suicide.
Despite those gaps in treatment, Phoenix maintains a broad spectrum of public and private services: AHCCCS expansion, community behavioral health clinics, 24/7 crisis teams, peer support networks, and expanding access to medication-assisted treatment (MAT).
For individuals in need of professional, evidence-based treatment, The Haven Detox – Arizona provides comprehensive addiction and mental health care serving residents of Phoenix and surrounding Maricopa County communities. This guide explains how to access addiction, mental health, and substance use services in Phoenix, helping readers navigate a complex but robust treatment system.
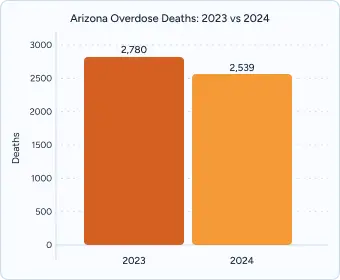
In 2023, Arizona recorded 2,780 drug overdose deaths across all substances. By 2024, that number had dropped to 2,539 deaths, reflecting an 8.7% decline from the previous year.
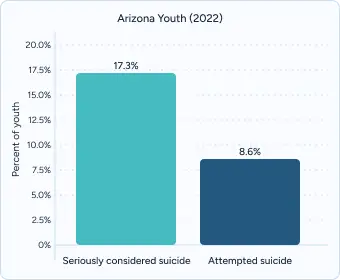
According to the Arizona Youth Survey 2022, 17.3% of youth reported having seriously considered suicide, and 8.6% reported a suicide attempt.
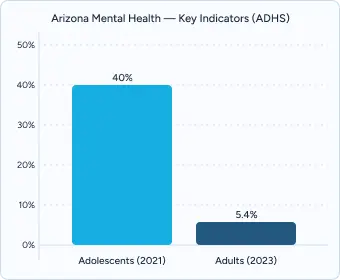
The Arizona Department of Health Services (ADHS) adolescent mental health report indicates that in 2021, about 40% of Arizona adolescents reported poor mental health during the COVID-19 pandemic.
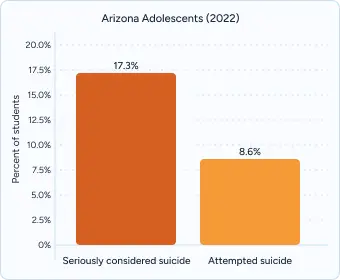
Data from the Arizona Youth Survey reveal that nearly one in five students reported suicidal ideation, while 8.6% attempted suicide. These rates are significantly higher among LGBQ+ youth, female students, and adolescents in economically disadvantaged districts.
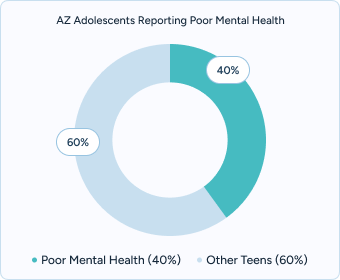
The Arizona Department of Health Services’ 2024 adolescent mental health report found that two out of five teens reported persistent feelings of poor mental health during the COVID-19 pandemic. Female and LGBQ+ students experienced disproportionately higher rates, highlighting critical disparities in access to care.

The Phoenix Health Department and partner agencies serve as centralized access points for treatment information and referrals. The City’s Phoenix Substance Use & Overdose Dashboard offers real-time data on suspected and fatal opioid overdoses, including demographic breakdowns (age, sex, ZIP code) and locations of overdoses.
Crisis intervention is available 24/7 via mobile crisis teams operating throughout Maricopa County. Connections Health Solutions in Phoenix completes psychiatric evaluations, 23-hour observation, and crisis stabilization for individuals with mental health or co-occurring substance use crises. After stabilization, they connect people with ongoing care such as outpatient programs, community resources, or residential treatment providers.
Mind 24-7 Clinics offers psychiatric walk-in services and emergency mental health treatment for co-occurring disorders in Phoenix.
Transportation accessibility supports connection to treatment programs across Phoenix. Public transit routes, including major bus lines, connect neighborhoods to behavioral health centers, crisis stabilization units, and outpatient clinics. Information from the Phoenix Department of Public Health includes a directory of crisis hotlines, treatment centers, and locations with 24/7 walk-in intake clinics.
The Arizona Health Care Cost Containment System, or AHCCCS, serves Phoenix residents seeking addiction and behavioral health care. This Medicaid Agency provides comprehensive coverage, which includes crisis intervention, outpatient therapy, residential services, medication-assisted treatment, and supports like peer recovery coaches, family services, case management, interpreter services, and transportation assistance when necessary.
The Arizona Health Care Cost Containment System has detailed policy standards for the timeliness of appointments and no-wait lists for covered behavioral health services:
Valleywise Behavioral Health Center in Maryvale, is a 24/7 acute behavioral health hospital and community emergency department with 192 beds, serving people of all ages.
Valle del Sol’s Maryvale Community Health Center provides behavioral health services, including psychiatric evaluation, medication management, counseling, and youth-focused transition-age programs. Walk-in appointments are available at some locations.
Non-profit clinics like CPLC Maryvale Community Service Center serve people with co-occurring mental health and substance use concerns in outpatient and rehabilitation settings, offering therapies like family counseling, trauma-informed treatment, group therapy, and psychosocial rehabilitation.
The Haven Detox – Arizona accepts most major insurance plans—including AHCCCS/Medicaid—and provides transportation assistance for individuals traveling from nearby areas. To learn more about programs and admissions, call the 24/7 helpline at (520) 614-1800 for personalized help.
Stand Together and Recover (S.T.A.R.) Centers operate multiple peer-run clubhouses in the Valley (Phoenix, Glendale, Avondale, Surprise), offering free, trauma-informed, member-driven programming. Services commonly include one-on-one peer support, groups, life-skills and employment coaching, social connection, and help navigating treatment or benefits. S.T.A.R. reports having served more than 120,000 Arizonans since its founding, and each location’s page lists hours, contact information, and programming so residents can find the nearest fit quickly.
Peer-involved crisis options are available at RI International’s Peoria Recovery Response Center and its on-campus Crisis Respite program, which blend clinical stabilization with peer support. These sites provide rapid walk-in access, 24/7 crisis care, short-term residential respite (13 beds at the Peoria campus), and connections to ongoing services once immediate risk has been addressed.
For people specifically looking for peer-run organizations, AHCCCS (Arizona’s Medicaid program) recognizes and lists peer- and family-run providers statewide and notes members’ right to request services from them. Health plans such as Arizona Complete Health also maintain current peer-run provider lists and explain how to access those services. These directories are useful when you want care delivered by staff with lived experience.
Arizona Recovery Housing Association (AzRHA) is a directory that helps Phoenix residents to find NARR-affiliated, AzRHA-certified recovery residences that meet statewide quality and safety standards (code of ethics, inspections, and operational criteria). AzRHA reports representing more than 1,600 certified recovery beds across Arizona, with many homes concentrated in metro Phoenix.
What to expect: certified homes typically maintain house rules that support sobriety (e.g., meeting participation, chores, drug/alcohol screening, curfews), offer peer support and accountability, and coordinate with outpatient treatment or mutual-aid meetings. The Arizona Recovery Housing Association (AzRHA) and National Alliance for Recovery Residences (NARR) outline these expectations and standards publicly, so prospective residents and families can compare options with consistent criteria.
There are a variety of recovery meetings to attend in the Phoenix area.
For Alcoholics Anonymous (AA), the Valley of the Sun/Greater Phoenix Intergroup maintains a live meeting directory with filters for day, time, format, and accessibility, and it feeds the national AA Meeting Guide app. Residents can search by neighborhood (e.g., Maryvale, Central City, North Phoenix) and find in-person or online options.
For Narcotics Anonymous (NA), the Arizona Region of NA provides a statewide meeting finder (including Phoenix-area listings), printable schedules, and a helpline. The regional site also lists Spanish-language meetings and Arizona-based virtual options, which can help when transportation or schedules are limited.
If you’re seeking identity-affirming and language-specific groups (e.g., LGBTQ+ or Spanish-speaking), both the AA Intergroup directory and the Arizona NA meeting finder include tags/filters and speaker lists where available, making it easier to match meetings to personal preferences and needs.
Comprehensive Assessment includes a full evaluation of substance use history, mental health conditions, and family systems. Programs connected with EMPACT-SPC, Banner Behavioral Health, and other AHCCCS-contracted providers typically include psychiatric evaluation alongside addiction screening to create individualized care plans.
Evidence-Based Therapies that utilize research-backed approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing (MI).
For individuals managing both substance use and mental health disorders, dual diagnosis treatment provides integrated support that addresses both conditions simultaneously.
Personalized treatment plans are developed through collaboration between clients and clinicians, reflecting individual goals, health needs, and social supports.
Medication-Assisted Treatment (MAT) – available through AHCCCS providers and private centers, offering buprenorphine (Suboxone), naltrexone (Vivitrol), and methadone when clinically appropriate, combined with counseling.
Cultural Competency is critical in Phoenix’s diverse population. Residents can look for programs offering Spanish-language services through bilingual staff and Latino-focused recovery groups in Maryvale and Alhambra. Traditional Indigenous healing practices are integrated into care, often coordinated with tribal health services in Maricopa County.
Evidence-Based Clinical Services include trauma-informed care and mindfulness-based relapse prevention, with staff maintaining ongoing clinical certifications and specialized training in co-occurring disorders.
Alumni and Peer Networks support long-term recovery through quarterly alumni reunions and digital peer forums connecting graduates with ongoing community support systems.
Administrative Support Services provides insurance navigation and sliding-scale financial consultations, with dedicated benefits advocates and care coordination specialists.
Programs that start aftercare planning during treatment see measurable, sustained improvements compared with treatment-only approaches. Strong continuing-care models involve scheduled check-ins, relapse-prevention coaching, stepped-down therapy, and rapid return to care if risk rises.
Family therapy and education can improve engagement, reduce use, and support safety planning. Ask about family therapy options and how your team will support healthy boundaries if family involvement isn’t safe or desired.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Insurance verification in Phoenix is supported by AHCCCS-contracted health plans, including Mercy Care and Arizona Complete Health. These programs review member benefits, determine eligibility for financial assistance, and connect uninsured residents with Maricopa County–funded behavioral health services. Case managers often assist with prior authorization requirements, ensuring that residents can begin treatment with minimal administrative delays.
Most facilities in Phoenix provide same-day comprehensive evaluations, followed by individualized treatment recommendations. Community organizations such as Solari Crisis & Human Services and RI International’s Recovery Response Center focus on warm handoffs between crisis stabilization services and appropriate community-based follow-up care, connecting individuals to outpatient providers, peer support programs, or other resources. These facilities maintain active communication with families, referring physicians, and social service agencies to support treatment readiness and strengthen long-term engagement.
Most Phoenix programs schedule intake assessments within 48 hours, but actual therapy start dates can vary depending on provider capacity. Many AHCCCS-contracted Community Behavioral Health Centers (CBHCs) offer same-day walk-in evaluations, and some private facilities can provide same-day or next-day admission when clinically appropriate. This helps reduce delays during crisis situations.
Yes. AHCCCS covers individual, family, and group therapy for eligible members, and most sessions have no out-of-pocket costs. Arizona Complete Health and Mercy Care also extend behavioral health coverage for children and adults, including medication management and crisis services. Copayments for behavioral health have been eliminated for AHCCCS members, removing financial barriers to access.
Phoenix has a large Latino community, and many peer support meetings and treatment programs offer bilingual services. The Arizona Hispanic Chamber of Commerce and local community centers host Spanish-language NA and AA meetings. Several Community Behavioral Health Centers (CBHC) and nonprofit providers employ native Spanish-speaking counselors and group facilitators to ensure cultural responsiveness.
Yes. Nonprofit clinics such as La Frontera Center provide sliding-scale therapy based on income, while SAMHSA block grants support no-cost crisis services for uninsured residents. Individuals can also apply for Arizona’s Behavioral Health Safety Net programs for assistance with outpatient and residential treatment.
Valley Metro provides discounted passes for low-income riders, and the RideChoice program offers subsidized rides for individuals with disabilities. Some treatment programs partner with Uber Health or Lyft Concierge to provide vouchers so patients can attend appointments or access stabilization centers.
Arizona maintains a robust 24/7 crisis system. Residents can call the statewide line at 1-844-534-4673 or dial 988 for immediate suicide and crisis support. Mobile crisis teams in Maricopa County respond within the hour, on average, offering on-site evaluation, stabilization, and connection to ongoing care.
Yes. Family peer specialists—trained individuals with lived experience—offer confidential support and coaching. Programs like NAMI Arizona, Al-Anon, and community-based family workshops help loved ones navigate intervention planning and coping strategies.
Phoenix providers offer culturally grounded services, including Spanish-language counseling, Native American healing circles, and LGBTQ+-affirming groups. Organizations such as Native Health Phoenix and one-n-ten serve Indigenous and LGBTQ+ communities with tailored mental health programming.
Yes. Peer-led youth recovery circles operate through organizations like Peer Solutions and the Teen Lifeline network. Colleges such as Arizona State University and Maricopa Community Colleges partner with behavioral health providers to run student-focused wellness programs. Specialized groups for 18–25-year-olds emphasize career readiness, identity support, and relapse prevention.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!