Melbourne Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
Melbourne, Florida faces significant mental health and addiction challenges, with Brevard County’s suicide rate of 20.7 deaths per 100,000 residents far exceeding both the Florida state average of 14.1 and the national rate of 14.0. Despite these concerning statistics, the city offers a comprehensive network of treatment resources, crisis intervention services, and recovery support systems designed to serve individuals and families across all neighborhoods and socioeconomic levels.
The treatment landscape includes both public and private options, with Florida Medicaid covering over 4 million residents and providing coverage for medically necessary addiction treatment services. Melbourne’s behavioral health infrastructure spans from immediate crisis response through mobile teams to long-term residential treatment, supported by Central Florida Cares Health System’s coordination of services throughout Brevard County.
This guide brings together recent statistics, youth mental health trends, local treatment infrastructure, and crisis resources. It also highlights what to look for in professional treatment and how programs like The Haven Detox – Florida provide safe, comprehensive care in a supportive setting for Melbourne Residents.
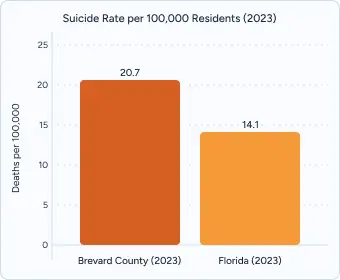
Melbourne and Brevard County face elevated mental health challenges compared to state and national averages. Recent 2023 data from the Florida Department of Health shows Brevard’s suicide rate at 20.7 deaths per 100,000 residents, representing a 47% increase over the Florida state average of 14.1 per 100,000. This alarming disparity places mental health intervention as a critical community priority.
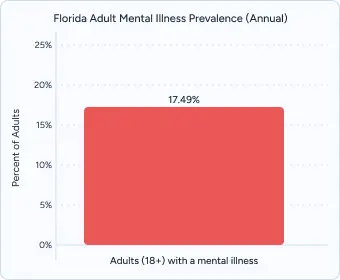
Florida leads the nation in adult mental illness, with 17.49% of adults—nearly 3 million residents—experiencing a diagnosable condition each year. Among youth aged 12–17, 15.51% report at least one major depressive episode annually, yet 61.80% of these adolescents receive no mental health services. Locally, Brevard County mirrors these high prevalence rates, underscoring the urgent need for expanded support in Melbourne and its surrounding communities.

In Brevard County, 15.9% of adults couldn’t see a doctor in the past year due to cost in the 2017–2019 period—only a slight improvement from 16.9% in 2016. Over the same span, the share of adults reporting poor mental health on 14+ days in the past month rose from 14.0% (2016) to 15.3% (2017–2019). Acute substance-use burden also remains substantial: Brevard saw 2,000+ non-fatal overdose emergency-department visits in 2021, and EMS responded to 3,050 suspected overdoses in 2023 (including 1,259 opioid-related). Together, these indicators point to persistent unmet need for timely, affordable mental-health and SUD care across the county.
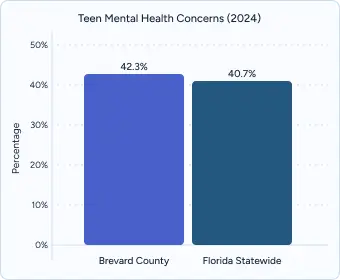
Recent data show Melbourne and the broader Brevard County area facing high rates of youth emotional distress. In 2024, 42.3% of Brevard County students reported feeling depressed or sad most days; the statewide rate was 40.7% (FYSAS). Nationally, fewer than half of adolescents with a major depressive episode receive treatment, underscoring major gaps in access to care.

In Brevard County, about one-third (33.5%) of middle and high school students reported feeling so sad or hopeless for two weeks that they stopped doing usual activities (2024). Statewide high-school data show girls report these feelings nearly twice as often as boys (51.6% vs. 27.3% in 2021), highlighting the need for targeted outreach and equitable resources so all young people can access care when they need it.

Central Florida Cares Health System coordinates access to outpatient, intensive outpatient, residential treatment, and medication-assisted treatment across Melbourne. Harm-reduction efforts support local naloxone availability through clinics, hospitals, and community organizations.
The Mobile Response Team (MRT) provides 24/7 crisis intervention, deploying licensed clinicians countywide to homes, schools, hospitals, and community sites to de-escalate crises and help families remain stable.
Transportation accessibility connects residents to care. While public transit is limited, many programs coordinate ride assistance, and the proximity of multiple Melbourne facilities helps reduce travel barriers.
Florida Medicaid provides comprehensive addiction treatment coverage for eligible residents, including medical detox, residential care, outpatient programs, and medications such as buprenorphine and naltrexone. As of July 2020, Medicaid eliminated copayments for substance use disorder treatment, with coverage available to residents up to 300% of the federal poverty level.
Statewide Managed Care updates expand access. Florida’s Medicaid program completed re-procurement in 2024, with new health plan contracts beginning in early 2025. Covered behavioral health services include assessments, evidence-based therapies, recovery support, case management, crisis services, short-term residential treatment, inpatient and ambulatory detox, intensive outpatient treatment, partial hospitalization, and mobile response teams.
Financial assistance reduces cost barriers. Many programs use sliding-fee scales based on income, and community health centers offer integrated primary care and behavioral health with discounted fees to help individuals receive care regardless of ability to pay.
Private insurance varies by plan. Benefits, networks, and out-of-pocket costs differ widely. Florida residents are more likely to face out-of-network mental health care than primary care, which can increase costs—checking benefits and obtaining prior authorizations can help minimize surprises.
Medicaid eligibility changed in 2024. Following the end of COVID-19 continuous coverage, Florida’s “Medicaid unwind” reassessed eligibility for millions of enrollees, and some individuals lost coverage. If your coverage changed, you may still qualify under a different category or program; check eligibility regularly, and update your information as needed.
If you’re looking for private care without long waits, Melbourne-area facilities can arrange quick intake and free insurance checks. These centers typically provide a full clinical assessment, medically managed detox when appropriate, and evidence-based therapies including CBT, trauma-focused treatment, and medication-assisted care.
Benefits of private programs compared over state-funded options often include:
Many programs secure insurance authorization within 24 hours and can coordinate same-day admission when it’s clinically appropriate.
At The Haven Detox – Florida, patients have immediate access to medical detox, residential rehabilitation, and dual diagnosis care in a safe and supportive environment. Treatment integrates proven therapies such as cognitive-behavioral therapy (CBT), group counseling, and relapse-prevention education with holistic wellness options like yoga & mediation or recreational activities that restore balance to daily life.
The West Palm Beach location features 24/7 medical monitoring, ensuring comfort and safety throughout detox and treatment. With a high staff-to-client ratio, the facility emphasizes individualized care in a restorative setting, offering modern amenities including chef-prepared meals, fitness spaces, and outdoor recreation to support whole-person healing.
The Haven Detox – Florida accepts most major insurance plans, including Medicaid and private carriers. Transportation support is available to remove barriers to treatment, helping patients from across Florida and beyond begin recovery without delay.
Care you can reach close to home. Across Brevard County, people can find support for depression, anxiety, trauma, and co-occurring substance use. Services range from psychiatry and talk therapy to psychological testing, telehealth visits, and integrated behavioral health within primary care. Many clinics offer bilingual providers, evening appointments, and income-based discounts to keep care affordable.
Neighborhood networks that meet local needs. School-connected counseling, community clinics, and university training centers expand low-cost therapy, while mobile crisis teams and same-day evaluation sites provide round-the-clock help during emergencies. Programs are designed with cultural responsiveness and family involvement in mind, and care teams coordinate with substance use treatment when both conditions are present.
Recovery Connections of Central Florida in Melbourne (downtown Melbourne, 1101 W. Hibiscus Blvd.) offers peer-led recovery coaching, sober social activities, and employment readiness support. The program also hosts family education nights and maintains an active online presence to keep the recovery community connected.
Brevard Peer Support Network in Palm Bay (250 Community Circle Drive) provides groups focused on mental health, substance use, parenting, and life skills. Services are free of charge, culturally responsive, and open to all ages. The center emphasizes accessibility, with transportation assistance available for those without reliable transit.
Neighborhood-based peer meetings across Brevard County are held daily in Melbourne, Cocoa, and Titusville, offering support tailored to local communities. Meetings include a mix of peer coaching, fellowship gatherings, and family support groups, with flexible hours on weekdays and weekends to ensure broad accessibility.
The Sober Pad (Melbourne/Rockledge) provides FARR-certified men’s sober living in professionally managed homes with structure, curfews, meeting participation, and peer accountability. Locations span Brevard County, including Melbourne, Palm Bay, Satellite Beach, and Rockledge.
Atlantic Beach Sober Living (Melbourne & Indian Harbour Beach) offers men’s recovery residences emphasizing community, accountability, and routine. Expectations include weekly rent and intake fees, curfews, random alcohol/drug testing, and attendance at outside recovery meetings.
The Glass House (Melbourne/Melbourne Beach) — women’s sober living provides a safe, supportive home exclusively for women, with structured routines and required participation in 12-step meetings to sustain long-term recovery.
Space Coast Area NA (spacecoastna.org) maintains an updated directory of Narcotics Anonymous meetings across Brevard County, with daily in-person and online options in Melbourne, Palm Bay, Cocoa, and Titusville. The schedule also syncs with the Meeting Guide mobile app, connecting residents to thousands of NA meetings nationwide.
Brevard Intergroup of Alcoholics Anonymous (aaspacecoast.org) organizes hundreds of AA meetings weekly throughout the county. Locations include Melbourne, Cocoa Beach, and Merritt Island, with formats ranging from open speaker meetings to step studies. The site provides newcomer resources, hotline support, and printable meeting schedules.
Spanish-language AA meetings are available in Brevard County, supported by bilingual volunteers and regional AA Español networks. These groups provide accessible support for the county’s Latino community through both in-person and virtual formats.
Specialty fellowship meetings offer focused support for diverse needs, including women’s groups, LGBTQ+ supportive meetings, young people’s recovery groups, and dual-diagnosis meetings that integrate mental health and substance use support. Many groups meet in hybrid formats, offering flexible access for individuals balancing work, family, or transportation challenges.
The best programs begin with a thorough intake that looks at substance use, mental health, medical history, and social supports—so care fits the person, not the other way around. Look for:
High-quality centers offer medication-assisted treatment (MAT) when appropriate—using FDA-approved options such as buprenorphine (Suboxone), naltrexone (Vivitrol), and methadone—and pair them with counseling, skills groups, and relapse-prevention planning.
Trust programs that uphold national standards, employ licensed clinicians, and provide 24/7 medical coverage during detox and stabilization. Culturally responsive care matters too—seek services in your preferred language, family-inclusive programming, and options tailored to your community.
Recovery continues after residential or outpatient care. Strong programs build individualized aftercare that may include therapy or IOP, peer-support connections, housing resources, and family education—so support follows you home.
Seamless handoffs and follow-through begin while treatment is still underway. Care teams line up next steps—outpatient therapy or IOP, peer-support meetings, sober housing, and community resources—so there’s no gap after discharge. Warm introductions and shared care plans help people stay connected as needs change over time.
Families as partners in recovery strengthen outcomes. Programs should offer family therapy, education on addiction and mental health, and support groups. Guidance focuses on healthy communication, setting boundaries, and knowing how to respond during setbacks—so loved ones can support recovery without enabling.
Proven therapeutic approaches such as CBT, DBT, trauma-focused counseling, and care for co-occurring conditions form the backbone of effective treatment. Leading facilities emphasize ongoing staff training and the use of current, evidence-based practices to deliver safe and consistent results.
Lifelong connections and ongoing support extend recovery well beyond discharge. Alumni programs, peer-led groups, and continuing care services give individuals a network to rely on when new challenges surface months or years later.
Guidance with insurance and benefits helps reduce barriers to treatment. Dedicated staff assist clients in navigating coverage rules, securing authorizations, and making the most of available insurance so care continues without unnecessary delays.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Most programs can confirm insurance benefits within 24 hours. Financial specialists help explain coverage, outline potential out-of-pocket costs, and review payment options so there are no surprises.
When treatment is needed, speed matters. Many facilities offer immediate assessments and can admit clients the same or next day, ensuring care begins without unnecessary delays.
Intake timelines vary by service type and individual needs. Many outpatient and intensive outpatient programs offer appointments within one week. Crisis intervention teams are available 24/7 for immediate support, and emergency departments provide on-the-spot care for urgent medical or psychiatric situations. Residential treatment facilities often schedule assessments within a few days, with the goal of minimizing wait times whenever beds are available.
Yes. Florida Medicaid covers medically necessary addiction treatment services at 100% for eligible enrollees. Covered services include medical detoxification, inpatient and residential programs, outpatient counseling, medication-assisted treatment (buprenorphine, naltrexone, methadone), and crisis intervention. Eligibility extends to individuals up to 300% of the federal poverty level, and copayments for substance use disorder treatment were eliminated in July 2020.
Several providers coordinate culturally responsive and bilingual care throughout Brevard County. Services include Spanish-language counseling, multilingual peer support groups, and family education sessions adapted to different cultural norms. Community health centers also offer sliding-scale fees and partner with local organizations to ensure programming addresses the needs of diverse communities.
Yes. While public transit is limited, many programs offer ride coordination, shuttle services, or transportation vouchers for clients. Some community clinics and health centers provide door-to-door transport for eligible participants. It’s recommended to inquire about transportation assistance when scheduling your intake appointment.
Crisis support is available around the clock. You can dial 988 to connect with the Suicide & Crisis Lifeline, which provides immediate counseling and referral services. Licensed mobile crisis teams respond to urgent situations in homes, schools, and community settings 24/7. Local emergency departments also have psychiatric and overdose stabilization capabilities at all hours.
Absolutely. Family members can access counseling, peer-support groups, and educational workshops independently. Crisis services can provide consultation on managing safety concerns, boundary-setting strategies, and legal options when a family member poses a risk to themselves or others. Support organizations such as Al-Anon also offer specialized guidance for families.
No one is turned away for inability to pay. Many community health centers and treatment programs operate on sliding-fee scales, and some offer payment plans or self-pay options. Crisis services and lifeline supports are free and confidential for all residents, regardless of insurance or documentation status.
Yes. Several clinics and wellness programs provide dedicated tracks for adolescents and young adults, offering age-appropriate group therapy, skills training, and academic support referrals. Universities and school districts also partner with local behavioral health agencies to facilitate access for enrolled students.
Your initial visit will involve a comprehensive assessment of your medical history, mental health status, substance-use patterns, and social supports. You’ll be asked to provide identification, insurance information, and any relevant medical records. The provider will discuss treatment recommendations, next steps, and scheduling for follow-up sessions or services before you leave.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!