Puerto Rico Addiction and Mental Health Treatment Resource Guide
Puerto Rico’s behavioral health landscape has been strained by hurricanes, earthquakes, and the COVID-19 pandemic. Approximately 70,000 individuals struggle with substance use, while one in four residents lives with a mental health condition—including 18% with anxiety and 10% with severe depression. Crisis calls to ASSMCA’s PAS hotline surged from 170,000 in 2019 to over 900,000 in 2020, underscoring the island’s urgent need for accessible, coordinated care.
Despite these challenges, Puerto Rico offers a range of treatment options through government agencies, community clinics, and private providers. This guide compiles verified statistics, state and municipal resources, and evidence-based pathways—empowering individuals and families to navigate the system and secure the support they need.
Need Professional Treatment Today? The Haven Detox – Puerto Rico provides immediate access with medical supervision for safer, more comfortable withdrawal management and comprehensive mental health care.
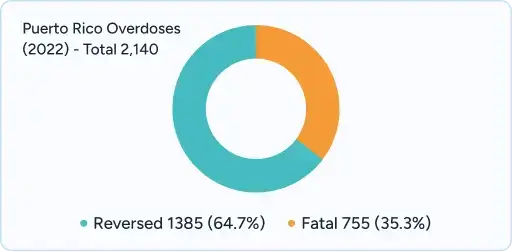
Puerto Rico recorded 2,140 overdoses in 2022, with 1,385 (64.7%) reversed by prevention programs and 755 fatal overdoses
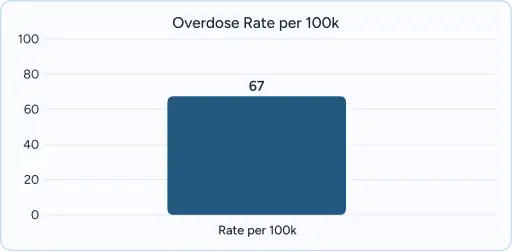
The island experiences 67 overdoses per 100,000 inhabitants – a rate of roughly one overdose every 4 hours
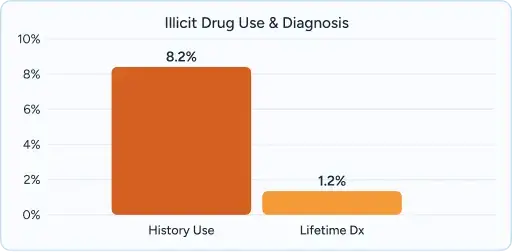
An estimated 8.2% of the population has a history of illicit drug use, with 1.2% qualifying for lifetime diagnosis of drug abuse or dependence

Heroin accounts for 43.5% of Puerto Rican addiction treatment admissions versus 13.2% for other Hispanics, indicating significantly higher rates of opioid addiction
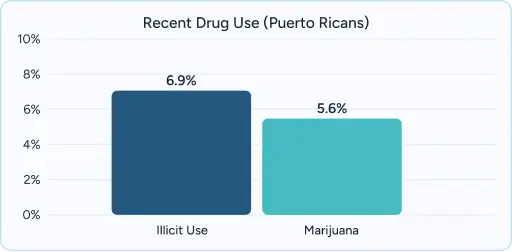
Puerto Ricans have the highest rate of recent illicit drug use (6.9%) and recent marijuana use (5.6%) among Hispanic subgroups
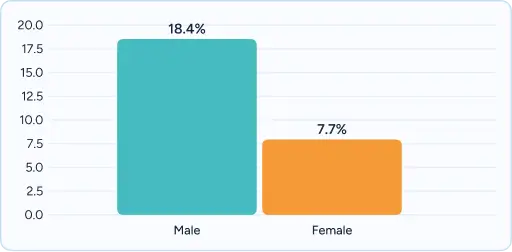
Male drug users are more than twice as likely to meet abuse criteria (18.4%) compared to females (7.7%)
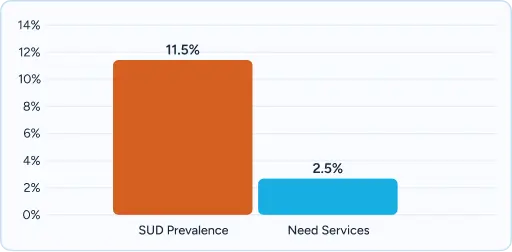
11.5% of adults aged 18–64 meet criteria for substance use disorder in the past 12 months, with 2.5% needing substance use services (57,301 adults).
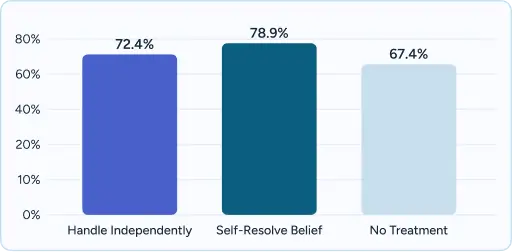
67.4% of adults needing substance services do not receive treatment, with top barriers including belief the problem would resolve itself (78.9%) and wanting to handle problems independently (72.4%).
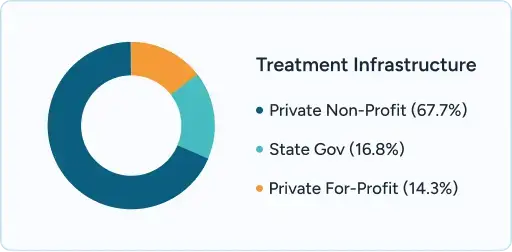
Treatment infrastructure includes 15,169 clients served across 67.7% private non-profit, 16.8% state government, and 14.3% private for-profit facilities.

32 facilities provide Medication-Assisted Treatment (MAT) as of 2023, with only 2 syringe exchange programs operating island-wide.
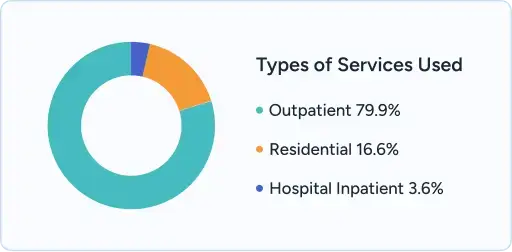
79.9% of clients receive outpatient services, 16.6% residential services, and 3.6% hospital inpatient care.

| Waiting Times | Long waiting lists and extended delays |
| Provider Availability | Limited provider availability, especially in rural areas |
| Funding Constraints | Funding constraints may limit service duration and intensity |
| Administrative Burden | Administrative complexity and paperwork hurdles |
| Quality and Standards | Variable quality and inconsistent standards across regions |
| Service Scope | Narrow scope of services and limited access to holistic care options |
| Withdrawal & Dual Diagnosis | Limited capacity for advanced withdrawal management; co-occurring disorders often treated separately |
| Therapy Approach | Standardized, less individualized therapies; limited access to advanced treatment modalities |
| Waiting Times | Same-day admission and 24/7 intake capability |
| Provider Availability | Extensive network of accredited, specialized providers |
| Funding Constraints | Comprehensive funding supports flexible, long-term care |
| Administrative Burden | Dedicated insurance specialists streamline prior authorization |
| Quality and Standards | Joint Commission, CARF, or similar accreditation ensures uniform high quality |
| Service Scope | Wide range of evidence-based therapies and holistic programs (e.g., art, music, yoga) |
| Withdrawal & Dual Diagnosis | Advanced withdrawal management and integrated dual diagnosis treatment capabilities |
| Therapy Approach | Evidence-based therapeutic modalities including specialized trauma-focused therapies |
Puerto Rico has become a central destination for addiction and mental health treatment, drawing both its 3.2 million residents and individuals from the U.S. mainland seeking culturally attuned, Spanish-language care. Across all 78 municipalities, patients can access a full spectrum of services—from specialized psychiatric hospitals and medication-assisted treatment programs in San Juan, Ponce, and Mayagüez to intensive outpatient clinics in Caguas, Bayamón, and Mayagüez. Rural satellite facilities extend essential counseling and support services to remote communities. Puerto Rico’s well-maintained highway network and intercity bus routes provide straightforward ground access, while Luis Muñoz Marín International Airport in San Juan and regional airports in Ponce and Aguadilla ensure direct connections for off-island patients.
Estimates indicate that up to 15 percent of patients in private treatment facilities travel from Florida, New York, Connecticut, New Jersey, and other neighboring states to benefit from Puerto Rico’s family-centered, community-based recovery models. Programs integrate outdoor therapeutic activities—such as beach-side mindfulness exercises, rainforest retreats, and equine therapy—with evidence-based clinical care, leveraging the island’s tropical climate and distance from mainland stressors. Treatment providers collaborate closely with U.S. counterparts to maintain continuity of care during and after transitions back home, ensuring that individuals and their families receive ongoing support. With its comprehensive service offerings, convenient transportation links, and a bilingual, bicultural workforce, Puerto Rico stands out as a supportive, accessible hub for long-term recovery from addiction and mental health challenges.

Understanding Puerto Rico’s complex insurance landscape can be overwhelming, particularly when navigating the intersection of Plan Vital Medicaid, Medicare Platino for dual-eligible individuals, and private insurance supplemental coverage. The managed care system requires coordination between multiple organizations, each with different authorization requirements, provider networks, and coverage limitations. Professional treatment centers recognize these challenges and provide dedicated insurance verification specialists who work directly with Plan Vital MCOs, private insurers, and federal programs to ensure seamless coverage verification and prior authorization when required. These patient advocates help families understand their benefits, identify covered services, navigate appeals processes, and coordinate with insurance case managers to prevent treatment delays. This support is particularly valuable for individuals requiring intensive services or those transitioning between levels of care, ensuring that insurance barriers do not prevent access to life-saving treatment.
25+ centers statewide providing free services through community-based organizations and ASSMCA-contracted providers:
While Puerto Rico offers excellent public resources, professional treatment facilities provide distinct advantages when immediate care is needed:
Recovery from addiction and mental health challenges is not only possible but achievable with the right support and professional intervention. Professional treatment offers genuine hope for long-term recovery, providing the medical expertise, therapeutic interventions, and comprehensive care coordination necessary for sustainable healing. In Puerto Rico, where 67.4% of adults needing substance abuse services do not receive treatment, choosing professional care becomes even more critical for breaking through barriers and accessing the evidence-based treatments that can transform lives and restore hope for individuals and families affected by behavioral health conditions.
Verify benefits and understand your treatment options
If you or a loved one is experiencing a mental health or substance use crisis, help is available right now:
Private treatment facilities typically offer same-day admission for both addiction and mental health crises, with 24/7 intake capabilities and no waiting lists. State-funded facilities through ASSMCA may have longer wait times, particularly for specialized services, with psychiatric appointments averaging 6-8 month delays. Emergency services are always available immediately through Línea PAS and hospital emergency departments.
Yes, Plan Vital (Puerto Rico’s Medicaid program) covers behavioral health services at contracted private facilities. The program operates through four managed care organizations (First Medical, MMM Multi Health, Triple-S Salud, and Plan de Salud Menonita) that coordinate with private treatment centers. Coverage includes detoxification, residential treatment, outpatient services, medication-assisted treatment, and mental health services without requiring primary care referrals.
Out-of-state residents can access treatment in Puerto Rico, and many facilities specialize in serving stateside Puerto Ricans seeking culturally competent care. Private insurance plans often provide coverage for treatment in Puerto Rico as it’s considered domestic care within the U.S. healthcare system. Patients should verify their specific insurance coverage and coordinate with facilities regarding travel arrangements and continuity of care planning.
Puerto Rico follows integrated treatment approaches for co-occurring disorders, with 93% of clients served having both conditions addressed simultaneously. ASSMCA requires facilities to provide coordinated mental health and substance abuse services, often in the same location. Treatment centers use evidence-based practices like Integrated Dual Diagnosis Treatment, combining psychiatric medication management with addiction counseling and behavioral therapies.
Puerto Rico has involuntary commitment statutes for individuals who pose imminent danger to themselves or others due to mental illness or substance use. Family members can petition the court system for emergency mental health evaluation and treatment. For substance use disorders, involuntary commitment is more limited and typically requires evidence of immediate physical danger. Most successful interventions involve professional intervention specialists and voluntary treatment engagement.
Most professional treatment centers offer alumni programs with ongoing support, including relapse prevention groups, individual counseling, and readmission services. Many facilities provide step-down care options and intensive outpatient programs for individuals who experience relapse. ASSMCA’s community programs also offer ongoing recovery support through peer specialists and case management services to prevent treatment discontinuation.
Treatment duration varies by individual needs and level of care. Detoxification typically lasts 3-7 days with medical supervision. Residential treatment ranges from 30-90 days, with some programs extending longer for complex cases. Intensive outpatient programs generally last 3-6 months with gradual step-down to regular outpatient care. Long-term recovery support through peer programs, alumni services, and community resources can continue indefinitely based on individual needs and preferences.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!