Mesa Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
Mesa has emerged as a focal point in Arizona’s opioid and behavioral health crisis, with Mesa West among the top Primary Care Areas for non-fatal opioid overdoses in 2023 (171 incidents statewide among PCAs). In 2023, Mesa West had some of the highest numbers of non-fatal opioid overdoses in the state. Across Arizona, there were about 54 overdoses for every 100,000 people, showing how widespread the problem is throughout Maricopa County.
Opioid deaths have stopped rising but remain very serious — nearly 2,000 people died from opioid overdoses in 2023, with fentanyl causing most of those deaths.
Mesa’s treatment and prevention infrastructure includes outpatient and inpatient programs, mobile crisis teams, peer support networks, and widespread distribution of overdose reversal tools such as naloxone. However, disparities in access remain: uninsured residents, those in higher-overdose zones like Mesa West, and historically underserved populations face greater barriers to prompt, sustained care.
For individuals in need of professional, evidence-based treatment, The Haven Detox – Arizona provides comprehensive addiction and mental health care serving residents of Mesa and surrounding Maricopa County communities. This guide provides residents with detailed pathways to addiction, mental health, and recovery services in Mesa, helping you identify care options suited to your needs and location.
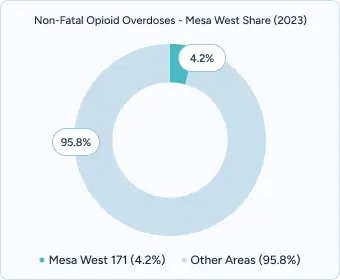
Arizona recorded 4,081 non-fatal opioid overdose events in 2023—a statewide rate of 54.2 per 100,000 residents. Within this landscape, Mesa West ranked among the highest-impact Primary Care Areas with 171 non-fatal overdose events, accounting for ~4.2% of the statewide total. These figures highlight the ongoing need for timely outreach, overdose education, and linkage to evidence-based treatment across Mesa.
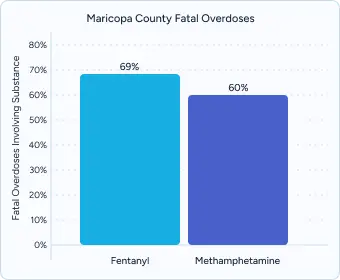
In Maricopa County, fatal overdoses most commonly involve fentanyl (~69%) and methamphetamine (~60%). These percentages overlap, meaning many deaths include both substances—an indicator of increasing polysubstance risk in Mesa and neighboring parts of Phoenix. Targeted harm-reduction (naloxone, test strips) and integrated treatment that addresses opioid and stimulant use together are essential.
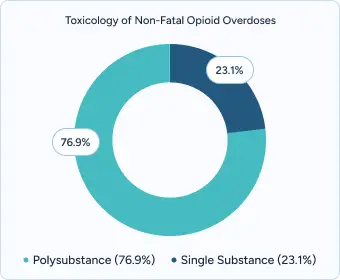
Toxicology from a 2021 review of non-fatal opioid overdose cases found 76.9% of people tested had two or more drugs in their system, compared with 23.1% with a single substance. This pattern reinforces the need for comprehensive screening, medication-assisted treatment, and coordinated behavioral health supports that reflect real-world polysubstance use in Mesa.
In Arizona, about one in six adolescents (ages ~12-17) experienced a major depressive episode in the past year.
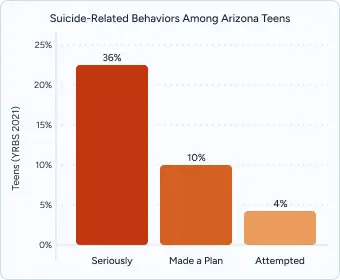
According to the Arizona Youth Risk Behavior Survey (YRBS) 2021 data from the Arizona Department of Health Services, about 23% of teens reported seriously thinking about suicide in the past year, 10% said they had made a suicide plan, and 4% reported a suicide attempt.

Mesa residents can access behavioral health and addiction treatment through AHCCCS-contracted Community Behavioral Health Centers (CBHCs), outpatient clinics, and crisis stabilization services. The AHCCCS Covered Behavioral Health Services Guide (CBHSG) outlines standards for services, including crisis intervention, residential treatment, intensive outpatient programming, therapy options, and peer support services statewide.
Mobile crisis teams operate throughout Maricopa County, providing 24/7 responses, in-person stabilization, and coordination with emergency departments. These teams work to reduce wait times for acute crises and help transition people from crisis to ongoing care. While Mesa West’s specific data are not reported separately, Maricopa County recorded more than 12,000 non-fatal overdose hospital visits in 2021, underscoring the significant need for timely crisis services.
Transportation access is variable but improving: many treatment facilities are accessible by Valley Metro routes, and some plans/providers now include supportive transportation services (e.g., for covered members who lack reliable means). The AHCCCS behavioral health service matrix includes “transportation” as a covered support service in many Behavioral Health Plans under certain medical necessity criteria.
The Arizona Health Care Cost Containment System (AHCCCS) covers treatment for addiction and mental health under Medicaid expansion, including medical detox, residential treatment, outpatient counseling, and medication-assisted treatment (MAT) such as buprenorphine, methadone, and naltrexone. Coverage extends to residents up to 138% of the federal poverty level, ensuring access to essential care.
For individuals not eligible for AHCCCS, state-funded programs provide sliding-scale fees, naloxone distribution, and other support services through community health centers and nonprofit organizations. These programs ensure broader access to treatment for residents who might otherwise fall outside Medicaid eligibility.
Community-based organizations in Mesa offer multilingual enrollment support, application navigation, and hands-on guidance to help residents access treatment. These local navigation programs provide outreach in English, Spanish, and other languages, ensuring families can complete paperwork, verify eligibility, and connect with appropriate services quickly.
Private treatment facilities in Mesa streamline entry into care, offering rapid insurance verification, same-day assessments, and individualized treatment planning. Facilities often provide enhanced privacy, holistic support options such as yoga and nutrition services, and evidence-based therapies like CBT and DBT.
The Haven Detox – Arizona serves Mesa and surrounding areas with 24/7 medical detox, dual-diagnosis support, and GeneSight® genetic testing to personalize medication management. Most major insurance plans, including AHCCCS, are accepted.
Mesa’s diverse mental health resources include hospitals, outpatient clinics, and school-based programs. Services are culturally responsive, offering Spanish-language therapy, trauma-informed practices, and supports for LGBTQ+ individuals and families.
Programs such as Resilient Health provide therapy, peer mentoring, and group support, while Casa de los Niños integrates trauma-focused care for children, youth, and families across the city’s schools, reinforcing access to long-term recovery pathways.
East Valley AA/NA coordinates support through the East Valley Intergroup office at 1320 E Broadway Rd, offering over 150 weekly meetings across Mesa and surrounding areas via online app partnerships.
Spanish-speaking AA groups serve Mesa’s Hispanic/Latino community through multiple locations, including Unity Church (2740 E Southern Ave) and St. Matthew’s Methodist (2540 W Baseline Rd). Meetings provide culturally responsive support with native Spanish-speaking sponsors, family programming, and connections to bilingual treatment resources.
Mesa Alano Club recovery meetings operate daily programming at 145 E 1st Ave, featuring morning meetings, evening support groups, and weekend social activities. Known for comprehensive Big Book study sessions, newcomer orientation programs, and partnerships with local treatment centers for continuing care coordination.
Effective treatment begins with a comprehensive assessment that evaluates both substance use history and co-occurring mental health conditions. In Mesa, programs are increasingly using integrated dual-diagnosis evaluations and family systems assessments to identify root causes and design tailored recovery plans.
Evidence-based therapies remain central to long-term success. You can often find services like:
Culturally responsive care is particularly critical in Mesa’s diverse community. Local providers integrate Spanish-language counseling, Native American healing practices (including sweat lodges and talking circles), and LGBTQ+ affirming therapeutic environments, ensuring that treatment reflects both cultural values and individual needs.
Aftercare coordination strengthens long-term recovery through comprehensive community connections.
Recovery is not limited to inpatient or outpatient treatment. In Mesa, quality programs emphasize aftercare planning from the first day of treatment, connecting clients with outpatient therapy, mutual aid groups, and sober housing. This warm handoff approach reduces the risk of relapse and ensures continuity of care.
Family engagement and support are integral to long-term recovery. Multi-family therapy groups, parent education workshops, and culturally tailored services, such as Spanish-language support sessions and Native American family healing circles, help ensure that recovery is supported at home as well as in treatment settings.
Mesa programs increasingly deliver integrated treatment models, addressing substance use disorders and mental health conditions simultaneously. This includes structured psychiatric care, medication management, and therapy designed for those with complex trauma or PTSD.
Trauma-informed care often incorporates EMDR and other trauma-focused therapies, with specialized training and supervision for counselors to ensure quality delivery.
Alumni support networks also play an important role, with many Mesa facilities hosting quarterly alumni events, digital peer support forums, and mentorship opportunities that allow graduates to maintain accountability and connection.
Finally, case management to help clients to help handle life outside of treatment like housing, FMLA, and job searching. Benefits advocates assist with insurance enrollment, AHCCCS applications, and sliding-scale fee arrangements, ensuring that recovery is accessible regardless of income or insurance status.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Immediate support and assessment services help Mesa residents begin recovery without delay. Individuals can access rapid placement into treatment through both public and private providers across Maricopa County.
Mesa residents benefit from insurance verification support through AHCCCS health plans such as Mercy Care and Arizona Complete Health. These programs confirm member benefits, assess eligibility for financial assistance, and connect uninsured individuals to county-funded treatment options.
Most Mesa facilities offer same-day comprehensive evaluations, followed by personalized treatment recommendations. La Frontera Center’s Mesa programs focus on “warm handoffs” from crisis stabilization to outpatient and community-based services, helping individuals stay engaged in care. Providers often coordinate with families, schools, and referral agencies to support engagement and readiness for treatment.
Most AHCCCS-contracted providers aim to schedule an initial behavioral health assessment within 48 hours of first contact, depending on clinical urgency. Some private providers, such as The Haven Detox – Arizona, can often provide same-day evaluations and next-day placement if medically appropriate, helping patients avoid waitlists.
Yes. Several organizations host Spanish-language AA/NA meetings and culturally responsive family therapy programs. Locations include Valleywise Health community clinics and local churches in West Mesa, ensuring access for Latino residents. Many peer-support circles also provide bilingual facilitators.
Yes. Nonprofit clinics such as Valleywise Health and federally qualified health centers (FQHCs) provide treatment on a sliding-scale fee basis. In addition, state-funded programs and SAMHSA grants help cover treatment for uninsured residents. Valleywise Health’s Mesa campus (480-344-2100) is a good starting point for financial navigation.
Yes. Valley Metro offers reduced-fare passes for eligible residents, while many treatment centers provide bus vouchers or ride coordination for patients. AHCCCS health plans may also cover non-emergency medical transportation (NEMT) to ensure clients can access care.
The 988 Suicide & Crisis Lifeline and the Arizona Statewide Crisis Line (1-844-534-4673) operate 24/7. Mobile crisis teams are dispatched throughout Mesa to provide on-site stabilization, overdose support, and referrals to ongoing care.
Yes. Family peer specialists offer confidential coaching and navigation services through programs supported by NAMI Arizona and Mercy Care. Families can also connect to Al-Anon meetings or intervention planning services to receive guidance when a loved one is not ready for treatment.
Mesa providers offer Native American healing circles, Hispanic/Latino family therapy programs, LGBTQ+-affirming recovery groups, and faith-based support options. This ensures culturally competent care tailored to diverse East Valley communities.
Yes. Several community-based organizations run college-age peer mentorship programs, sober social events, and groups designed for emerging adults ages 18–25. These programs focus on school stress, identity development, and preventing relapse during life transitions.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!