
Dr. Rostislav Ignatov, MD
Chief Medical Officer
Clonidine is a non-opioid medication for high blood pressure. In opioid or alcohol withdrawal, it’s used to calm the body when withdrawal makes your heart rate, blood pressure, and anxiety spike. By easing symptoms like sweating, shaking, restlessness, and a racing heart, clonidine can make early withdrawal more manageable.
Clonidine does not treat opioid or alcohol cravings and does not treat substance use disorders directly. It’s a support medication sometimes added to make the most intense phase of withdrawal more manageable.
Table of Contents
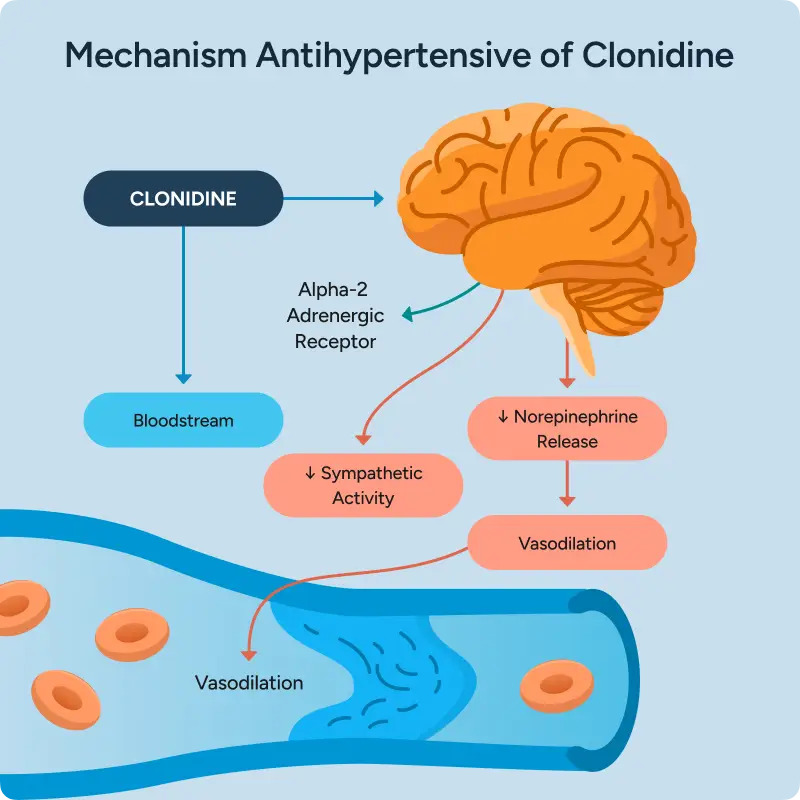
Opioid or alcohol withdrawal causes a surge in stress chemicals that overstimulate the nervous system.
Clonidine works by reducing this stress signaling. It activates alpha-2 adrenergic receptors in the brain and nervous system, which act like feedback brakes. When these receptors are activated, the brain releases less norepinephrine, the chemical that drives the fight-or-flight response.
With fewer stress signals being sent:
This is why clonidine can reduce the physical intensity of withdrawal even though it does not act on opioid or alcohol receptors. Clonidine may also help with nausea, gastrointestinal discomfort, and tremor associated with sympathetic over activation.
Important: Clonidine does not reduce cravings and does not replace medications that treat opioid or alcohol dependence. Its role is calming the body’s stress response during acute withdrawal.
| Before Clonidine | After Clonidine |
| Withdrawal triggers excess norepinephrine release | Alpha-2 receptors are activated |
| Stress signals flood the nervous system | Norepinephrine release is reduced |
| Heart rate and blood pressure rise | Stress signaling slows |
| Sweating, agitation, and restlessness increase | Physical withdrawal symptoms ease |
Clonidine is limited by blood pressure and heart rate, which is why it’s used carefully and alongside other medications rather than as a primary treatment.
In detox, clonidine is used to reduce physical withdrawal stress—not to sedate or “knock someone out.”
A typical approach includes:
Decisions about clonidine use and dosing are made by medical providers based on symptoms and vital signs, not a fixed protocol. If clonidine isn’t enough on its own, other medications are added rather than increasing clonidine beyond safe limits.
Clonidine can be given as a pill or, less commonly, as a patch. In most detox settings, pills are used because dosing can be adjusted quickly as symptoms and blood pressure change.
Patches release clonidine slowly over several days and are used less often during acute detox, when flexibility and close monitoring are important.
Most patients describe clonidine as taking the edge off the physical stress of withdrawal. Many notice reduced anxiety, less internal agitation, and a calmer body state.
| What It Should Feel Like | What It Should Not Feel Like |
| Less restlessness or agitation | Feeling faint or unable to stand |
| Reduced anxiety | Excessive sleepiness or confusion |
| Alert and aware | Feeling “out of it” |
In detox settings, clonidine is considered a comfort medication because it helps control the physical stress response of withdrawal. Comfort medications don’t replace treatment for opioid use disorder, but they play an important role in reducing unnecessary distress so the body can stabilize during early withdrawal.
No. Clonidine does not cause a “high,” euphoria, or intoxicated feeling. It does not act on opioid or alcohol receptors and does not produce the effects people associate with addictive drugs.
Most people describe clonidine as calming rather than mind-altering. If clonidine causes excessive sleepiness, dizziness, or feeling mentally foggy, that usually means the dose needs adjustment or isn’t the right fit. The medical team monitors for this and makes changes as needed.
Opioid withdrawal pushes the body into a constant “fight-or-flight” state. Heart rate rises, blood pressure increases, and the nervous system stays stuck on high alert. This is why withdrawal can feel so intense and unrelenting.
Clonidine works by calming that overactive stress response. Even though it’s classified as a blood pressure medication, its role in detox is to quiet the nervous system—not to treat high blood pressure itself. By lowering the body’s stress signals, clonidine can reduce many of the physical symptoms that make withdrawal feel overwhelming.
This approach doesn’t replace opioid treatment or cravings support. It helps the body feel steadier while it moves through the hardest phase of detox.
Clonidine can begin helping within the first day or two, but its full benefit is usually judged over several days as withdrawal symptoms change.
What to expect:
Clonidine doesn’t work the same way for everyone. If it isn’t providing meaningful relief, the treatment plan is adjusted.
Clonidine stays in the body longer than its noticeable calming effects. For most people:
Because clonidine affects blood pressure and heart rate, it’s usually tapered rather than stopped suddenly once withdrawal symptoms improve. This helps prevent rebound symptoms like elevated blood pressure or increased agitation.
START
Take your last dose

72 HOURS
Physical symptoms at peak

1 WEEK
Physical symptoms start to lessen

2 WEEK
Psychological and emotional symptoms
1 MONTH
Cravings and depression

Most patients do not stay on clonidine after detox. It’s usually used short-term for comfort symptoms, then tapered down or stopped before discharge once anxiety, agitation, and physical withdrawal symptoms settle.
Stopping clonidine suddenly can cause rebound symptoms, including elevated blood pressure or increased agitation, which is why tapering is used when appropriate.
Clonidine can be helpful, but it doesn’t work the same way for everyone. Common reasons it may not provide enough relief include:
This does not mean detox is failing. It means the plan is being adjusted to better match what the body needs.
Clonidine lowers blood pressure and heart rate, which is why vitals are checked before dosing. If blood pressure is too low, a dose may be held. This is a routine safety decision, not a sign that detox isn’t working.
The most common side effects during detox include:
Less commonly, some people experience headache, constipation, or fatigue. Blood pressure and heart rate are monitored closely, and doses are adjusted as needed.
For most people in medical detox, clonidine is considered low risk when properly monitored. The main risks are related to how clonidine lowers blood pressure and slows the nervous system.
Clonidine requires extra caution for people who:
This doesn’t mean clonidine can’t be used, but it does mean closer monitoring or a different medication may be safer.
In a medical detox setting:
Because clonidine’s risks are dose-related and reversible, problems are usually prevented before they become serious.
Clonidine can sometimes be used alongside other blood pressure medications, but only with careful monitoring. Because clonidine lowers both blood pressure and heart rate, combining it with certain medications can increase the risk of dizziness, fainting, or an excessively slow heart rate.
Extra caution is needed for people taking beta-blockers. In these cases, clonidine may be avoided, used at lower doses, or replaced with other comfort medications. Decisions are based on the specific medication, dose, and how the body responds during detox.
Clonidine is sometimes used as part of an alcohol or opioid detox plan for people who need relief from the physical stress of withdrawal, especially when opioid-based medications aren’t the best option or aren’t preferred.
Clonidine is one option for calming the body’s stress response during withdrawal. Other medications may be used depending on symptoms and medical history, including:
Trying to push through opioid detox at home can turn dangerous fast.
Medical detox provides a safer, more closely monitored way to get through withdrawal. Symptoms are treated, vitals are monitored, and the plan can be adjusted minute-by-minute.
Most insurance plans cover detox and the medications used (including Clonidine).
Get answers about your cost / coverage now.
Your information will be kept private
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!