
Arizona Addiction and Mental Health Resources
When every moment counts, professional detox and psychiatric support are vital. In 2023, Arizona recorded 1,928 opioid overdose deaths—while the overall opioid fatality rate dipped slightly, synthetic opioids (primarily illicit fentanyl) were implicated in 97.6% of these deaths.
Behavioral health access remains limited: only 40.6% of adults with a diagnosable mental illness received services in the past year, and 27.4% of Arizonans who needed counseling or therapy could not obtain it, often due to cost and provider shortages.
Need Professional Treatment Today? The Haven Detox – Arizona delivers rapid admission, private treatment, around-the-clock medical monitoring for safer withdrawal, and integrated behavioral health care to address co-occurring disorders.
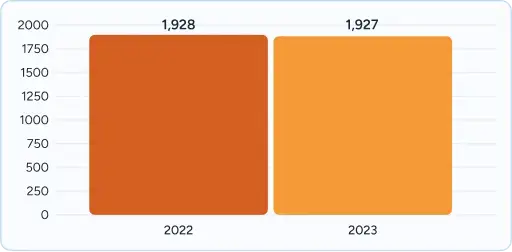
1,928 opioid overdose deaths in 2023 (virtually unchanged from 2022, suggesting a plateau after years of increases).
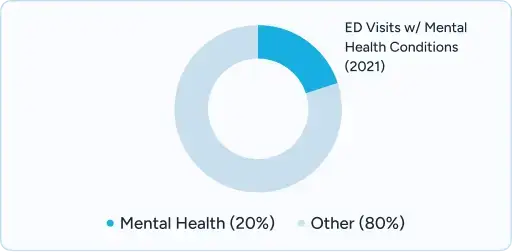
482,331 emergency department visits in 2021 involved mental health conditions — nearly 1 in 5 ED visits statewide.
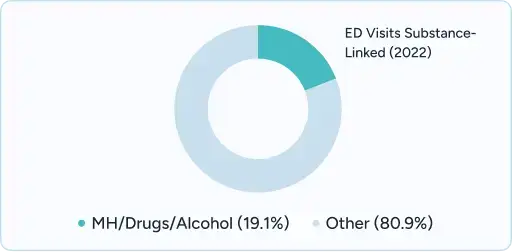
In 2022, 19.1% of all ED visits were tied to mental health, drugs, or alcohol.
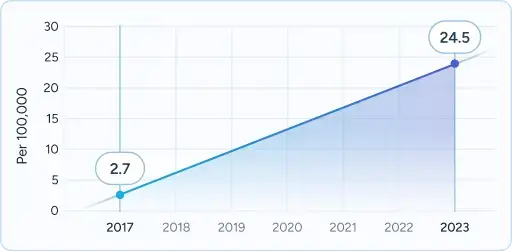
Native American overdose fatality rates rose 807% from 2017–2023 (2.7 → 24.5 per 100,000).

Black Arizonans’ overdose fatality rates more than tripled in the same period (12.5 → 41.9 per 100,000).

Arizona ranks 49th nationally for adult mental health care access.
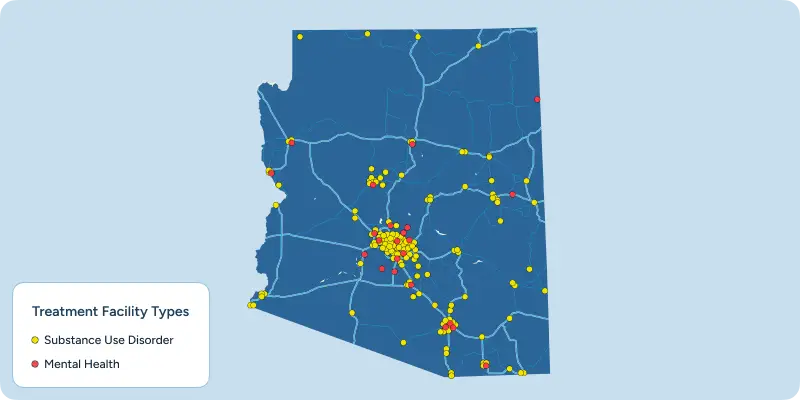
Arizona’s behavioral health system is broad but uneven. The state has built a strong crisis network with hotlines, mobile teams, and short-term stabilization units, but these services are meant only for brief stays before patients are moved elsewhere. Most inpatient psychiatric and residential treatment facilities are concentrated in the Phoenix metro area, which means rural and tribal communities often face longer travel times or even out-of-state placement.
Care is overseen by Regional Behavioral Health Authorities (RBHAs), which manage Medicaid-funded services such as detox, outpatient programs, and crisis stabilization. Access, however, varies widely by region, with some areas experiencing longer delays than others.
Community supports also play an important role. Peer specialists, drop-in recovery centers, and federally supported clinics (FQHCs and CCBHCs) help extend care to underserved populations. At the same time, supportive housing for people with Serious Mental Illness (SMI) remains severely backlogged, with many waiting years for placement.
Taken together, these layers form the backbone of Arizona’s treatment infrastructure — comprehensive in design but frequently stretched by high demand.
The Arizona Health Care Cost Containment System (AHCCCS) funds detox, residential, outpatient, and crisis services, coordinated through Regional Behavioral Health Authorities (RBHAs).
Arizona operates a statewide 24/7 crisis system, including hotlines, mobile crisis teams, and stabilization units coordinated through RBHAs. While this ensures a safety net, limited bed space means many behavioral health crises still end up in emergency departments.
Through AHCCCS, individuals may access certified Peer & Recovery Support Specialists (PRSS) who provide lived-experience support, coaching, and group engagement. Peer-run centers like S.T.A.R. Centers also operate across Arizona, offering drop-in services and community programs.
Arizona funds permanent supportive housing programs for members with serious mental illness (SMI) or co-occurring substance use disorders. These programs tie rental assistance with ongoing case management and behavioral health support, recognizing that stability in housing can improve recovery outcomes.
Through federal and state partnerships, the MHBG supports community mental health centers across Arizona. These centers deliver outpatient treatment, day programs, and emergency services in underserved communities — often filling gaps when local providers are at capacity.
CCBHCs in Arizona provide comprehensive behavioral health care, including substance use treatment, regardless of a person’s insurance status. Funded through Medicaid and federal SAMHSA grants, they aim to expand access in underserved areas.
Arizona’s FQHCs deliver integrated primary care, mental health, and substance use treatment for patients regardless of their ability to pay. These centers receive federal and state support to ensure access in rural and low-income areas.
As Maricopa County’s public safety-net hospital system, Valleywise Health operates three dedicated Behavioral Health Centers. These centers provide inpatient and crisis care and serve as a cornerstone of publicly funded treatment in the Phoenix metro area.
While Arizona has a wide safety net of outpatient and crisis services, there are limited options for high-acuity mental health care such as long-term residential or inpatient psychiatric programs. Most state-funded resources are focused on stabilization, outpatient therapy, and supportive housing.
This shortage means many individuals with serious, ongoing psychiatric needs still rely heavily on emergency departments or out-of-state placements to receive care.
| Residential Mental Health Care | |
| Length of Stay | |
| Medical Supervision | |
| Dual Diagnosis | |
| Admission Wait Times | |
| Geographic Reach |
| Residential Mental Health Care | |
| Length of Stay | |
| Medical Supervision | |
| Dual Diagnosis | |
| Admission Wait Times | |
| Geographic Reach |
AHCCCS provides a wide range of addiction treatment services for eligible residents. Coverage includes detoxification services, residential treatment, partial hospitalization (PHP), intensive outpatient programs (IOP), and outpatient counseling. Medication-assisted treatment (MAT) is also covered, including medications such as methadone, buprenorphine, and naltrexone to support safe and effective withdrawal and long-term recovery. Peer and recovery support services are integrated, offering guidance and advocacy from certified peers.
AHCCCS covers all medically necessary mental health services, including inpatient psychiatric stabilization, outpatient therapy, medication management, and crisis services. Preventive screenings, wellness checks, and ongoing psychiatric care are also included, with no cost-sharing for most programs. Members with serious mental illness (SMI) diagnoses receive access to additional supports, such as case management and supportive housing.
Several large private insurers provide coverage for addiction and mental health treatment in Arizona. Many professional treatment centers accept both AHCCCS and commercial plans, ensuring broad access to care. Major carriers include:
These insurers cover multiple levels of care, from detox to residential and outpatient programs. Coverage details vary by plan, so families are encouraged to verify benefits prior to admission.
Arizona has taken several policy steps to respond to the opioid epidemic and growing behavioral health needs:
Progress has been made, but Arizona still ranks 49th nationally for adult mental health access, highlighting the gap between policy and real-world care.
Comprehensive services offered through S.T.A.R. Centers and similar programs include:
Arizona certifies Peer & Recovery Support Specialists (PRSS) through AHCCCS-approved training:
Arizona regulates sober living homes through ADHS, with voluntary certification from the Arizona Recovery Housing Association (AzRHA):
NAMI Arizona operates regional affiliates and provides:
Finding help close to home can make a difference in recovery. The Haven Detox offers local addiction and mental health resource guides across Arizona, helping residents connect with community programs, treatment options, and peer support in their area.
When evaluating any treatment facility in Arizona, remain cautious of places that:
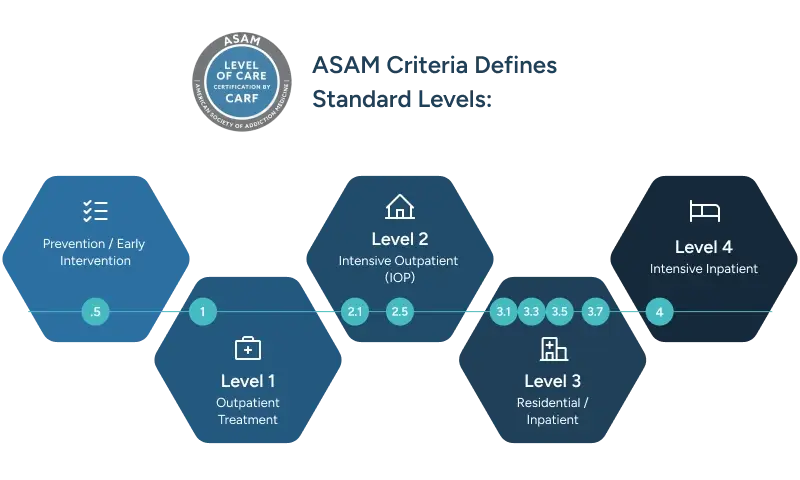
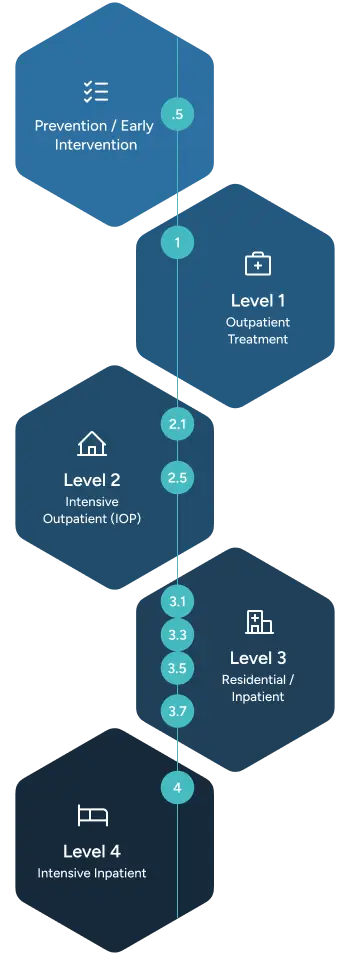
Highest ASAM level, hospital-based, with 24/7 physician management and nursing supervision.
Includes:
While Arizona offers important public resources through AHCCCS and RBHAs, professional treatment facilities provide distinct advantages when immediate, comprehensive care is needed:
Choosing the right level of care is critical. Arizona’s public system provides a foundation of access, but professional centers can often deliver the timeliness, medical excellence, and environment that families seek when facing urgent mental health or substance use crises.
Verify benefits and understand your treatment options
Compare programs, read reviews, and make informed decisions
If you or a loved one is experiencing a mental health or substance use crisis, help is available right now:
Yes. AHCCCS covers detox, residential, outpatient, peer support, and crisis stabilization for qualifying members. Those with a Serious Mental Illness (SMI) designation may also qualify for expanded services like case management and housing support.
Many professional facilities accept both AHCCCS and private/commercial insurance. Coverage varies by plan and level of care, so most providers recommend an insurance verification process before admission.
Residential programs in Arizona typically range from 30 to 90 days, though some state-funded programs provide shorter stays (2–4 weeks) focused on stabilization.
The majority are concentrated in the Phoenix metro area, particularly at Valleywise Behavioral Health Centers. Options are more limited outside Maricopa County, which can require travel for high-acuity care.
Yes. Tribal RBHAs coordinate AHCCCS-covered services for tribal members, and organizations like Native Health Phoenix and Seven Arrows Recovery offer programs blending traditional healing (ceremonies, talking circles) with clinical treatment.
Arizona offers 24/7 crisis hotlines and mobile crisis teams statewide. Professional facilities may also provide same-day admission, avoiding being constantly referred elsewhere to find a bed can occur in state-funded programs.
Options include:
Yes. Arizona requires sober living homes to be licensed by ADHS. Over 1,600 recovery housing beds are certified by the Arizona Recovery Housing Association (AzRHA), offering safe, structured environments with peer support.
Be cautious of programs that:
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!