Get Help Today 24/7
Glendale Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
The toll of addiction and mental health struggles is felt across families and neighborhoods, with fentanyl continuing to drive much of the crisis in Glendale. Yet within this challenge, there are signs of hope. Arizona recorded an 8.7% decline in overdose deaths from 2023 to 2024, reversing years of steady increases. Still, Maricopa County alone reported 1,554 overdose deaths in 2023—about 34.6 per 100,000 residents—showing that the work is far from over.
For Glendale residents, a full spectrum of care is available. Medical detox, residential programs, outpatient and intensive day treatment, medication-assisted treatment, and peer recovery supports are all within reach. Much of this care is coordinated through AHCCCS, which served more than 273,000 people with substance use services in 2024. Community partners such as Solari Crisis & Human Services answer calls around the clock, provide crisis response, mobile teams, and neighborhood outreach to help people connect with support right when they need it.
For individuals in need of professional, evidence-based treatment, The Haven Detox – Arizona provides comprehensive addiction and mental health care serving residents of Glendale and surrounding Pima County communities. This guide walks through how to access drug rehab and mental health treatment in Glendale and greater Maricopa County, making it easier to navigate a complex system and find the right next step toward recovery.
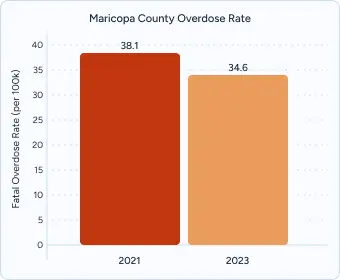
Maricopa County’s fatal overdose rate dropped from 38.1 per 100,000 residents in 2021 to 34.6 per 100,000 in 2023. While this marks progress from the recent peak, the county still recorded 1,554 deaths in 2023. Men are dying at nearly three times the rate of women (51.7 vs. 17.7 per 100,000), underscoring the need for targeted prevention and outreach.
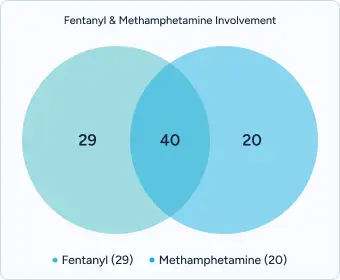
In 2023, fentanyl was present in 69 percent of overdose deaths countywide, while methamphetamine was detected in 60 percent. The overlap shows how often these substances are combined, creating a more dangerous and unpredictable drug supply that complicates treatment and recovery.
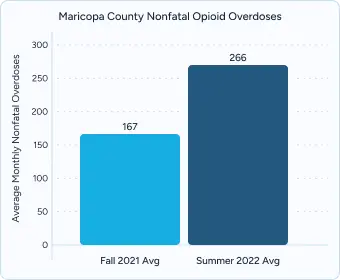
Between September 2021 and August 2022, Maricopa County reported 2,466 suspected nonfatal opioid overdoses. Monthly averages rose from about 167 in fall 2021 to 266 in summer 2022, keeping emergency responders and hospital systems under constant strain while highlighting the importance of stronger connections to ongoing care.
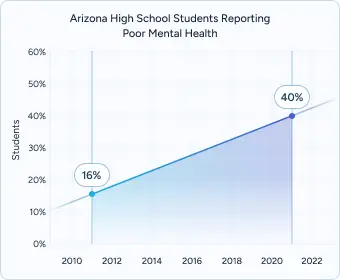
The share of Arizona high school students reporting poor mental health rose from about 16 percent in 2011 to nearly 40 percent in 2021. Female students reported much higher rates than males (51 percent vs. 22 percent), while LGBTQ+ students were even more affected (63 percent vs. 26 percent for heterosexual peers).

According to state-level NSDUH estimates, the percentage of Arizona youth ages 12–17 experiencing a major depressive episode increased from 9.5 percent (2004–2008) to 13.2 percent (2013–2017). These trends reflect a long-term rise in clinical depression among young people that has yet to level off.
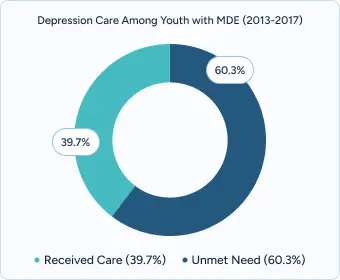
Even as more youth experience depression, only about 39.7 percent of those with a major depressive episode received depression care during 2013–2017. This treatment gap highlights the urgency of improving access to school-based mental health supports, culturally competent providers, and early intervention programs.

RI International’s West Valley Recovery Response Center operates a 24/7 walk-in crisis facility serving Glendale and the West Valley. The center provides on-scene evaluations, short-term stabilization, and peer-supported care to help individuals regain safety and connect with appropriate community services.
Glendale’s neighborhoods are connected to behavioral health and treatment facilities through Valley Metro bus routes and light rail service to downtown Phoenix. For residents with mobility challenges, the Valley Metro ADA paratransit (Dial-a-Ride) provides door-to-door transportation to medical and behavioral health centers, ensuring that lack of transit is not a barrier to care.
Despite these resources, Maricopa County continues to face a shortage of licensed clinicians compared to the national average. This shortage places additional pressure on crisis teams and outpatient programs, often leading to longer wait times. To help bridge the gap, many providers rely on peer specialists, nonprofit organizations, and private treatment centers, which expand capacity and improve access to timely care.
AHCCCS covers medically necessary care for eligible Glendale residents—including medical detox, residential treatment, partial hospitalization (PHP), outpatient programs (OP), peer support, and medication-assisted treatment (MAT) with buprenorphine, methadone, and naltrexone. Coverage extends to adults up to 138% of the federal poverty level. Many behavioral health copays are $0, and 24/7 crisis services are covered at no cost.
Integrated “Complete Care” plans (effective October 1, 2022) combine physical and behavioral health under a single plan. In Maricopa County, members commonly enroll with Mercy Care or Arizona Complete Health – Complete Care Plan, which coordinates crisis stabilization, outpatient therapy, case management, peer recovery, and serious mental illness (SMI) services. Apply through Health-e-Arizona PLUS or call 1-888-788-4408 for multilingual assistance, including Spanish.
If you’re not eligible for AHCCCS, Glendale’s community health centers and nonprofits can help. Many offer financial assistance, sliding-scale fees, and connections to naloxone and harm-reduction resources through county-funded opioid response programs.
The Haven Detox – Arizona, located in Green Valley, serves residents of Glendale and surrounding communities and accepts most major insurance plans, including AHCCCS/Medicaid, and offers transportation support for residents traveling from surrounding regions.
Private addiction treatment centers in Glendale and greater Maricopa County help reduce barriers to care by offering streamlined insurance verification, rapid intake assessments, and access to evidence-based therapies such as cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), and trauma-focused interventions. Many programs also integrate holistic services—like yoga, fitness, and nutrition—to support recovery on multiple levels.
Private facilities may provide advantages compared to state-funded programs, including:
Glendale residents benefit from a growing behavioral health network designed to meet the needs of diverse neighborhoods across the West Valley. Services range from outpatient therapy and crisis stabilization to integrated dual-diagnosis treatment, ensuring that individuals facing both mental health and substance use disorders can access coordinated care.
Glendale’s behavioral health resources are concentrated in key neighborhoods:
Stand Together And Recover (S.T.A.R.) Centers – Phoenix/Valley Locations
Serves Glendale residents with peer certification training, WRAP (Wellness Recovery Action Plan) facilitation, and recovery coaching. Programs combine in-person and virtual options, creating flexible access for individuals balancing work, school, or caregiving responsibilities.
Crisis Response Network Peer Warm Line (1-844-733-9912)
A statewide, 24/7 service staffed by trained peers with lived experience, providing emotional support and connections to crisis or treatment services. This program helps combat social isolation while offering practical recovery tools.
Arizona Recovery Housing Association (AzRHA)
Oversees state-certified recovery residences that meet National Alliance of Recovery Residences (NARR) standards. AzRHA maintains a searchable directory of certified homes to ensure quality and compliance.
Haven House Networks
Provides AzRHA-certified housing with 24-hour staff support, secure entry, Wi‑Fi, and community kitchens. Residents participate in weekly house meetings, chore rotations, and sobriety monitoring to build accountability and life skills.
Valley Recovery Residences
Holds NARR Level 2 certification and offers case management, transportation support, and employment services. Structured requirements include a 90-day minimum stay, weekly recovery meetings, and adherence to curfew and house guidelines.
Other transitional housing programs in Glendale include homes like Glendale Transitional Living / Transitional Home, Oxford House Sun Devil West, Oxford House Adsila, Oxford House Sunset Palms, among others. These residences vary in size (often 7–10 occupants), and generally require participation in meetings, drug screening, and adherence to house rules. These transitional housing options ensure Glendale residents have access to safe, structured environments that support long-term recovery and reduce the risk of relapse.
In Glendale, effective treatment begins with a complete assessment that looks at both substance use and mental health, since co-occurring disorders are common. Strong programs don’t just screen for addiction—they also consider psychiatric needs, trauma history, and family context, building a care plan that supports the whole person.
Glendale’s diverse population also means cultural responsiveness is essential. The best programs offer Spanish-language services and bilingual staff for the city’s large Hispanic and Latino community, incorporate practices that respect Native American cultural traditions, and provide LGBTQ+-affirming spaces that reduce stigma and help clients engage more fully in recovery.
Quality treatment typically brings together several core elements:
In Glendale, aftercare planning starts while treatment is still underway. Providers work to ensure warm handoffs into outpatient counseling, peer recovery groups, and transitional housing, so clients don’t face gaps in support once they leave a residential or intensive program. This kind of structured transition reduces treatment drop-off rates and helps people stay connected as they move back into their community.
Strong programs also recognize that recovery rarely happens in isolation. Glendale facilities often integrate families through multi-family therapy sessions and educational workshops that build understanding and trust. Spanish-language offerings and trauma-informed family circles are particularly important for Hispanic and Latino households, as well as families impacted by intergenerational trauma.
Together, these long-term strategies help reduce relapse risk, build resilience, and strengthen the community, making the recovery process more sustainable.
While support groups and community resources play an important role, professional treatment offers protections and opportunities that informal care simply can’t provide.
Trauma-Informed Care: Many Glendale facilities incorporate evidence-based trauma therapies, including Eye Movement Desensitization and Reprocessing (EMDR) and somatic experiencing techniques, delivered by clinicians with ongoing certification in trauma recovery.
Alumni and Peer Networks: Long-term support includes quarterly alumni events, digital recovery communities, and mentorship programs that connect current clients with individuals in sustained recovery.
Family Engagement: Structured family therapy and psychoeducation workshops strengthen support systems and reduce relapse risk.
Benefits Navigation: Dedicated staff assist with insurance verification, FMLA paperwork, and sliding-scale fee consultations, ensuring patients and families understand and can access available resources.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Glendale residents can get fast benefit checks—often within 24–48 hours—through AHCCCS-contracted plans such as Mercy Care and Arizona Complete Health or directly with participating programs. Teams confirm eligibility, estimate any out-of-pocket costs, handle prior authorizations, and connect uninsured residents to county-funded options when available.
Many Maricopa County providers offer same-day clinical assessments with next-day placement when beds are available and medically indicated. Community partners such as COPE Community Services and Solari’s navigation team emphasize warm handoffs between crisis stabilization, detox, residential, and step-down care, helping you begin treatment quickly and keep support continuous.
Most AHCCCS providers in Glendale, such as COPE Community Services, schedule intake assessments within 48–72 hours. Some community health centers also offer same-day walk-in evaluations when capacity allows, making it easier for residents to access timely care.
Yes. AHCCCS plans—including Arizona Complete Health and Mercy Care—cover medical detox, residential treatment, outpatient counseling, and medication-assisted treatment (MAT). As of 2024, most behavioral health copayments have been eliminated for eligible members.
Yes. Chicanos Por La Causa (CPLC) Behavioral Health Services offers bilingual peer-support meetings, and Alcoholics Anonymous maintains Spanish-language groups across West Valley locations. Services include native Spanish-speaking facilitators and culturally tailored programming.
Uninsured residents can access sliding-scale services at Mountain Park Health Center – Maryvale or through grant-funded programs supported by AHCCCS. Call the Arizona Statewide Crisis Line (1-844-534-4673) for navigation and financial assistance referrals.
Valley Metro offers reduced-fare passes, RideChoice, and paratransit services. Many Glendale treatment programs also provide transportation vouchers or mobile outreach teams for clients with mobility or financial barriers.
Crisis lines and mobile response teams are available 24/7. Call 988 for the Suicide & Crisis Lifeline or the Arizona Statewide Crisis Line (1-844-534-4673) for immediate mental health or substance-use assistance.
Yes. NAMI Valley of the Sun provides free family support groups, peer-led education programs, and coaching for loved ones navigating a mental health or substance use crisis.
Programs include Spanish-language groups through CPLC Behavioral Health, LGBTQ+-affirming services through one·n·ten Phoenix, and veteran-focused peer counseling through Be Connected Arizona, a statewide initiative linking veterans and families with resources.
Yes. Peer Solutions and one·n·ten partner with local campuses to offer peer mentoring, youth leadership programs, and mental health education workshops for students ages 18–25.
CDC. U.S. overdose deaths decrease almost 27% in 2024. CDC Newsroom. Published May 8, 2025. Accessed September 17, 2025. https://www.cdc.gov/nchs/pressroom/releases/20250514.html
CDC. Vital Statistics Rapid Release: Provisional drug overdose death counts. National Center for Health Statistics. Updated August 6, 2025. Accessed September 17, 2025. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
National Institute on Drug Abuse (NIDA). Overdose death rates. National Institutes of Health. Updated 2025. Accessed September 17, 2025. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
Arizona Department of Health Services. Opioid overdoses surveillance report, Arizona, 2023. ADHS. Published 2023. Accessed September 17, 2025. https://www.azdhs.gov/opioid/documents/opioid-report-2023.pdf
Arizona Department of Health Services. An update on Arizona overdose trends and ADHS actions. ADHS. Published May 7, 2025. Accessed September 17, 2025. https://www.domesticviolence.az.gov/sites/default/files/meeting-documents/materials/4._adhs_opioid_update.pdf
Arizona Department of Health Services. Youth Risk Behavior Survey—past results. ADHS. Updated March 21, 2024. Accessed September 17, 2025. https://www.azdhs.gov/yrbs/past-results.php
Arizona Department of Health Services. Adolescent mental health report. ADHS. Published 2024. Accessed September 17, 2025. https://www.azdhs.gov/documents/prevention/womens-childrens-health/adolescent-health/2024-adolescent-mental-health-report.pdf
Maricopa County Department of Public Health. Substance use data dashboard. Maricopa County. Updated 2024. Accessed September 17, 2025. https://www.maricopa.gov/5833/Substance-Use
Maricopa County Department of Public Health. Overdose data dashboard. Maricopa County. Updated May 14, 2024. Accessed September 17, 2025. https://www.maricopa.gov/6205/Overdose-Data
Substance Abuse and Mental Health Services Administration (SAMHSA). Key substance use and mental health indicators in the United States: Results from the 2023 National Survey on Drug Use and Health. HHS Publication No. PEP24-07-01-001. Published 2024. Accessed September 17, 2025. https://www.samhsa.gov/data/
Substance Abuse and Mental Health Services Administration (SAMHSA). Behavioral Health Barometer: Arizona, Volume 5. SAMHSA. Published 2023. Accessed September 17, 2025. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/Arizona-BH-BarometerVolume5.pdf
Substance Abuse and Mental Health Services Administration (SAMHSA). Substance use and mental disorders in the Phoenix-Mesa metro area. NSDUH Metro Brief Report. Published 2023. Accessed September 17, 2025. https://www.samhsa.gov/data/sites/default/files/NSDUHMetroBriefReports/NSDUH-Metro-Phoenix.pdf
Health Resources and Services Administration (HRSA). Health professional shortage areas data. HRSA Data Warehouse. Updated 2024. Accessed September 17, 2025. https://data.hrsa.gov
Arizona Health Care Cost Containment System (AHCCCS). Behavioral health services. AHCCCS. Accessed September 17, 2025. https://www.azahcccs.gov/Members/BehavioralHealthServices/
Arizona Health Care Cost Containment System (AHCCCS). Covered services. AHCCCS. Accessed September 17, 2025. https://www.azahcccs.gov/Members/AlreadyCovered/coveredservices.html
Arizona Health Care Cost Containment System (AHCCCS). AHCCCS health plans. Updated September 30, 2024. Accessed September 17, 2025. https://www.azahcccs.gov/healthplans
Arizona Health Care Cost Containment System (AHCCCS). Crisis hotlines. Behavioral Health Resources. Accessed September 17, 2025.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private


Why Wait?
Get Answers Now
You’re here because you know you need help. Let’s talk through it together. There’s no commitment and it’s 100% confidential even to check your insurance.
100% Confidential


Why Wait?
Get Answers Now
You’re here because you know you need help. Let’s talk through it together. There’s no commitment and it’s 100% confidential even to check your insurance.
100% Confidential