Fall River Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
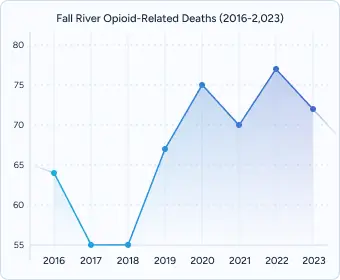
Fall River faces some of the state’s most urgent addiction and mental health challenges. In 2023, the city recorded one of Massachusetts’s highest overdose death rates — 76.6 per 100,000 residents — more than double the state average. Yet this same community distributes more naloxone per capita than almost any other city in the Commonwealth, reflecting both the urgency of the crisis and the strength of its recovery network.
This guide explains how to access addiction, mental health, and recovery services in Fall River, helping residents navigate a complex but resilient treatment system that blends public services, community support, and private care.
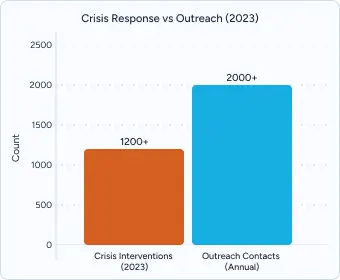


Fall River offers a layered network of behavioral health services that combine hospital care, community programs, and nonprofit organizations. Child & Family Services, located at 1052 Pleasant Street, serves as one of the city’s central access points for mental health support, providing crisis referrals and operating a 24/7 Mobile Crisis Intervention team. SSTAR continues to play a leading role in substance use and behavioral health treatment, offering both outpatient programs and harm reduction services that reach some of the city’s most vulnerable residents. At the hospital level, Southcoast Health’s St. Anne’s Hospital provides emergency psychiatric stabilization and links patients to longer-term care options, like the Haven Detox – New England.
Mobile crisis teams strengthen this infrastructure by responding to urgent situations within roughly an hour. These teams deliver in-home psychiatric evaluations, stabilization, and warm handoffs to appropriate treatment programs, offering a community-based alternative to emergency department boarding. Their presence reduces delays in access to care and helps de-escalate crises before they become medical emergencies.
Transportation remains a practical but important element of treatment access. Local routes through GATRA and SRTA connect neighborhoods with clinics and recovery centers, while MassHealth funds medical transportation to substance use appointments. The Gateway Link extends Fall River’s reach by connecting residents to treatment centers in Taunton and Brockton, ensuring that those needing specialized services are not confined to city limits.
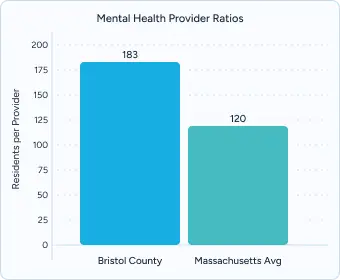
Despite these resources, challenges remain. Fall River has fewer licensed clinicians per capita than many other Massachusetts cities, a shortage that puts pressure on the system and increases reliance on peer specialists, nonprofit organizations, and private providers such as The Haven Detox. These gaps underscore both the need for immediate crisis response and the importance of building long-term treatment capacity across the region.
Recovery in Fall River is sustained by a strong network of peer-led centers, housing programs, and mutual aid groups. At the heart of this system are two dedicated recovery centers. The Fall River Recovery Connection Center, located at 649 Bedford Street, provides free peer-led services, including bilingual Spanish programming, trauma-informed workshops, and sober social events designed to build connection. Similarly, the Steppingstone Peer 2 Peer Recovery Support Center on Stanley Street offers one-on-one coaching, structured support groups like AA, NA, and SMART Recovery, and reports encouraging outcomes, with 85 percent of participants maintaining abstinence six months after engagement.
Safe and stable housing is another cornerstone of recovery. The Steppingstone Men’s Recovery Home, a MASH-certified Level II residence, provides 23 beds in a structured environment with 24/7 staffing, group meetings, and strict accountability measures. The Resilient Homes – Jordan Matthew House, accredited at Level II, offers transitional living with peer mentorship and sober accountability, balancing structure with greater independence. These programs ensure residents are surrounded by support while they rebuild their lives.
Mutual aid remains central to the community’s fabric. The Fall River Area Intergroup coordinates more than 45 AA and NA meetings each week, many hosted at churches and community centers across the city. For the city’s large Portuguese- and Spanish-speaking populations, bilingual meetings such as “Esperanza” provide culturally specific spaces for recovery and connection. Younger residents also benefit from peer-driven groups tailored to ages 18–25, which combine mentorship, job readiness workshops, and sober social activities to create healthier alternatives to substance use.
Together, these recovery supports highlight Fall River’s community action and strength: a city that meets people where they are, offering multiple entry points into sustained healing and long-term wellness.
MassHealth covers 100% of behavioral health and addiction treatment costs for qualified residents, including medical detox, residential treatment, outpatient therapy, and medications such as Suboxone, buprenorphine, and methadone. As of 2020, copayments for substance use disorder services have been eliminated, and eligibility extends to residents up to 138% of the federal poverty level.
For those not eligible for MassHealth, the Massachusetts Behavioral Health Partnership (MBHP) offers state-funded financial assistance for residents with incomes up to 300% of the federal poverty level. This program ensures that even households above the Medicaid threshold have a pathway to covered behavioral health care.
The Health Safety Net helps Fall River residents without insurance access treatment at local hospitals and community health centers. Many providers in the city are designated Safety Net locations, meaning that essential services — from emergency stabilization to outpatient therapy — remain accessible regardless of insurance status.
Residents can apply for coverage through the Massachusetts Health Connector, with applications and enrollment support available in Portuguese, Spanish, and Khmer, reflecting Fall River’s diverse population. Local community health centers and nonprofit agencies also provide hands-on navigation to help families complete paperwork, verify coverage, and connect with appropriate treatment.
Professional treatment centers offer urgent mental health and addiction needs. Residents can receive assessments, crisis stabilization, and referral to the appropriate level of care, all typically covered by MassHealth. While this system ensures no-cost entry points, the availability of residential beds or specialty services can mean waiting longer for placement.
Private treatment centers can shorten the time between asking for help and beginning care. By handling insurance checks quickly and coordinating intake directly, these programs help clients move from assessment into treatment with fewer delays.
Some advantages of private treatment options include:
The Haven Detox in Worcester provides 24/7 medical detox and dual-diagnosis care for clients with both addiction and mental health conditions. Evidence-based therapies include Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), alongside advanced tools like GeneSight genetic testing allowing for more personalized medication management.
With one of the highest staff-to-client ratios in Massachusetts, the facility near Fall River blends medical oversight with resort-style amenities, including catered meals, fitness areas, and transportation support statewide. Most major insurance plans, including MassHealth, are accepted, and admissions staff are available around the clock to guide residents and families through the process.
Effective treatment for addiction and mental health is never limited to detox alone. In Fall River and across Massachusetts, providers are expected to deliver continuity of care that spans from initial stabilization to long-term recovery supports. Comprehensive programs recognize that healing is not just clinical — it requires attention to medical needs, emotional well-being, family involvement, and community connection.
A full continuum of care often includes:
Research shows that programs lasting 90+ days improve long-term outcomes by up to 60%, and family therapy can reduce relapse risk by nearly 40%. Equally important, comprehensive programs provide warm handoffs into outpatient care, peer recovery centers, and housing, so clients leave treatment with clear supports already in place.
Fall River’s recovery community is anchored by dedicated peer-led centers where residents find both immediate support and long-term connection. The Fall River Recovery Connection Center, located at 649 Bedford Street, offers trauma-informed workshops, bilingual Spanish programming, and sober social events that help people rebuild their lives in community. On Stanley Street, the Steppingstone Peer 2 Peer Recovery Support Center provides one-on-one coaching, telephone support, and peer-led groups including AA, NA, and SMART Recovery. Outcomes are strong: 85% of participants report abstinence six months after engagement.
Stable housing is one of the most important building blocks of recovery. Fall River is home to several MASH-certified recovery residences, which provide structure, accountability, and a safe living environment. The Steppingstone Men’s Recovery Home offers 23 beds in a Level III certified program with 24/7 staff, house meetings, and random screenings. The Resilient Homes – Jordan Matthew House operates at Level II certification, balancing independence with peer mentorship and sober accountability. Both options ensure residents have a stable foundation while rebuilding their lives.
Mutual aid is a central part of Fall River’s recovery culture. The Fall River Area Intergroup coordinates more than 45 AA and NA meetings every week, spread across churches, community halls, and treatment centers. For the city’s Portuguese- and Spanish-speaking populations, bilingual meetings such as Esperanza offer culturally specific spaces for healing. Young adults ages 18–25 can access groups that combine recovery support with mentorship, job readiness, and sober social events, providing positive alternatives and strong peer networks.
Together, these programs reflect the commitment of Fall River’s recovery community: meeting people where they are, removing barriers to care, and ensuring that support does not end when formal treatment does. With peer coaches, recovery housing, and vibrant mutual aid, Fall River has built one of the strongest recovery ecosystems in Massachusetts.
Choosing the right treatment program can feel overwhelming, but there are clear signs that separate strong, trustworthy care from average or inadequate options. The best programs combine medical expertise, proven therapies, and long-term supports while also addressing the whole person and their family.
Every quality program should provide:
Every strong program begins with a complete evaluation of both substance use and mental health. Since most clients face overlapping challenges, dual-diagnosis treatment ensures nothing is overlooked and care can be matched to individual needs.
Lasting results come from proven approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Eye Movement Desensitization and Reprocessing (EMDR), and Motivational Interviewing. At The Haven Detox, these therapies are delivered alongside Family Therapy, which has been shown to lower relapse rates by nearly 40%.
Healing extends beyond clinical work. Quality care should include yoga, art therapy, Reiki, nutrition support, and mindfulness practices. The Haven Detox also offers GeneSight genetic testing, a cutting-edge tool that helps personalize medication plans for better outcomes.
Addiction and mental health affect entire families. Programs that include family education, group sessions, and ongoing support provide clients with a stronger foundation for recovery.
Treatment is only the first step. The best programs create a continuing care plan before discharge, including outpatient therapy, peer support, housing options, and access to alumni networks. These warm handoffs make transitions smoother and keep recovery momentum strong.
Trauma-Informed Care utilizes evidence-based approaches including EMDR and cognitive processing therapy, with specialized training required for all clinical staff providing trauma services.
Alumni Recovery Networks support long-term sobriety through quarterly virtual reunions and peer mentorship programs, maintaining connections between graduates and current clients through digital support platforms.
Benefits Navigation Services provide insurance advocacy and sliding-scale consultation assistance, employing dedicated financial coordinators and community resource specialists to ensure treatment accessibility.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Recovery begins with a single phone call or online inquiry.
Most facilities verify coverage within 24–48 hours, often providing preliminary information immediately. At The Haven Detox, financial counselors help families understand benefits, estimate out-of-pocket costs, and explore funding options when needed.
When clinically indicated, assessment and admission can happen rapidly. Many programs—including The Haven Detox—offer same-day evaluations and next-day admission, ensuring minimal delay between asking for help and starting treatment.
Community Behavioral Health Centers (CBHCs) provide same-day walk-in evaluations, while The Haven Detox offers same-day assessments and next-day admissions when medically appropriate.
Yes. MassHealth covers 100% of approved behavioral health services, including detox, residential treatment, outpatient care, and medications. If you’re not eligible, programs like MBHP and the Health Safety Net provide additional support.
Several Fall River programs offer state-funded slots, sliding-scale fees, and financial counseling. Haven provides insurance verification within 24–48 hours and will guide families through funding options for the uninsured.
Yes. Many providers in Fall River—including CBHCs, peer recovery centers, and support groups—offer bilingual Portuguese and Spanish clinicians, as well as interpreter services. Specialized groups like Esperanza provide culturally tailored support.
Absolutely. Family participation improves long-term recovery. Programs like The Haven Detox include Family Therapy, educational workshops, and support groups to rebuild trust and reduce relapse risk.
Recovery continues with aftercare planning that includes outpatient therapy, peer recovery centers, and MASH-certified sober housing. Haven maintains an Alumni Program to keep clients connected long after discharge.
Yes. Specialized services in Fall River address the needs of transitional-age youth (18–25) with peer mentorship, job readiness training, and young adult recovery groups.
The Haven Detox provides a range of evidence-based approaches including CBT, DBT, EMDR, and Motivational Interviewing. These therapies address both immediate symptoms and underlying causes of addiction and mental health conditions.
Massachusetts Department of Public Health. Opioid-Related Overdose Deaths by City/Town, MA Residents: 2012–2023. Boston, MA: Massachusetts Department of Public Health; 2024.
Massachusetts Department of Public Health. Opioid-Related Overdose Deaths, All Intents by City/Town, 2016–2023. Boston, MA: Massachusetts Department of Public Health; 2024.
Massachusetts Department of Public Health. Bureau of Substance Addiction Services Annual Report, 2023. Boston, MA: Massachusetts Department of Public Health; 2024.
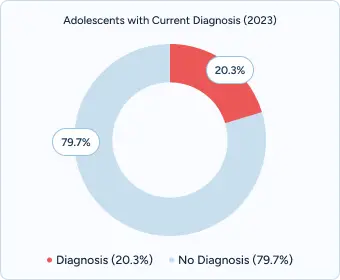
Substance Abuse and Mental Health Services Administration (SAMHSA). National Survey on Drug Use and Health: Detailed Tables, 2016–2023. Rockville, MD: SAMHSA; 2024.
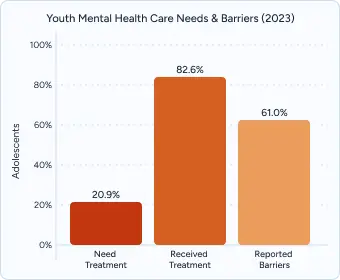
Massachusetts Department of Elementary and Secondary Education (DESE). Student Health Survey and Youth Risk Behavior Survey, 2019–2023. Malden, MA: DESE; 2023.
Annie E. Casey Foundation. Kids Count Data Center: Child and Youth Mental Health Indicators. Baltimore, MD: The Annie E. Casey Foundation; 2024.
Health Resources and Services Administration (HRSA). Area Health Resource File: Mental Health Provider Ratios by County, 2023. Rockville, MD: HRSA; 2023.
Massachusetts Behavioral Health Partnership. Member Handbook and Coverage Information. Boston, MA: MBHP; 2024.
Massachusetts Health Connector. Health Coverage Options for Massachusetts Residents. Boston, MA: Massachusetts Health Connector; 2024.
National Institute on Drug Abuse. Principles of Drug Addiction Treatment: A Research-Based Guide, 3rd ed. Bethesda, MD: National Institutes of Health; 2018.
Substance Abuse and Mental Health Services Administration (SAMHSA). Treatment Improvement Protocol 39: Substance Abuse Treatment and Family Therapy. Rockville, MD: SAMHSA; 2019.
Massachusetts Alliance for Sober Housing. MASH-Certified Sober Homes Directory and Standards. Boston, MA: MASH; 2024.
Steppingstone Inc. Annual Outcomes Report, Peer 2 Peer Recovery Support Center. Fall River, MA: Steppingstone Inc; 2023.
Massachusetts Behavioral Health Help Line. Accessing Crisis Services Across Massachusetts. Boston, MA: Commonwealth of Massachusetts; 2024.
Massachusetts Poison Control Center. Emergency Overdose Response and Naloxone Distribution. Boston, MA: Massachusetts Poison Control; 202.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!