
Dr. Rostislav Ignatov, MD
Chief Medical Officer
Drug and alcohol withdrawal can feel like a bad flu. Nausea, vomiting, sweating, chills, body aches, and exhaustion are common as the body adjusts. For some patients, nausea and vomiting become intense enough to interfere with fluids, nutrition, and other medications needed during detox.
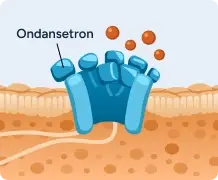
Ondansetron (Zofran) is an anti-nausea comfort medication used during medical detox to help control vomiting. It does not treat the substance use disorder directly, but helps patients feel more comfortable during detox so the body can stay stable while other detox medications do their work.
Table of Contents
Nausea and vomiting are common during opioid and alcohol detox, especially in the early days.
As the body adjusts to the absence of substances, strong nausea signals can travel from the gut to the brain. This can leave the stomach feeling constantly unsettled or lead to repeated vomiting.
Ondansetron is used as a comfort medication to help calm these nausea signals.
Ondansetron doesn’t stop withdrawal or speed it up. Its purpose is to reduce vomiting so the body can settle and the person can feel more physically comfortable during detox.
Ondansetron is often used early in detox, when stomach symptoms are most disruptive. When nausea is under better control, it becomes easier to:
Keeping up with these nutrition basics helps the body better self-heal, prevents complications, and allows other medications to work to work properly.
How Ondansetron (Zofran) Blocks Nausea Signals During Detox
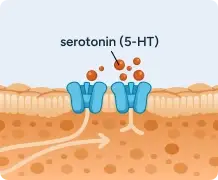
Withdrawal releases serotonin in the gut, activating 5-HT₃ receptors and sending nausea signals to the brain.
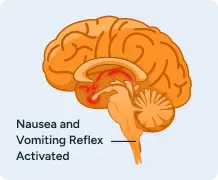
Serotonin activates 5-HT₃ receptors in the brainstem, triggering the vomiting reflex.
Withdrawal releases serotonin in the gut, activating 5-HT₃ receptors and sending nausea signals to the brain.
During withdrawal, the nervous system is under stress. This stress affects more than one system at a time, including the digestive tract.
That’s why detox can feel flu-like. Nausea, vomiting, chills, sweating, body aches, and exhaustion often show up together. These symptoms are uncomfortable, but they are a known part of the body adjusting to the absence of substances.
Comfort medications like ondansetron help ease specific symptoms while the body stabilizes.
During opioid and alcohol withdrawal, nausea is triggered by signals between the gut and the brain. One of the main chemicals involved in this process is serotonin. When the body is under stress, serotonin can activate the nausea reflex and lead to vomiting.
Ondansetron works by blocking these nausea signals. It interrupts the pathway that tells the brain to trigger vomiting, which helps calm the stomach without affecting alertness or mental clarity.
Because of how it works, ondansetron:
Its role is focused on comfort. By reducing nausea and vomiting, ondansetron helps the body better tolerate detox while other medications address withdrawal symptoms and safety concerns.
Nausea often peaks early during opioid or alcohol detox and improves as the body stabilizes. Timing varies based on the substance used, length of use, and overall health. Medical detox helps manage symptoms safely while they change.
Ondansetron is most often used during the early days of detox, when nausea and vomiting are more likely to show up. This usually happens within the first few days after opioids or alcohol are stopped, as the body reacts to the sudden change.
Not everyone going through detox needs ondansetron. It’s used when stomach symptoms start to interfere with basic care or make detox harder to tolerate.
During early withdrawal, the body is under a lot of stress. The nervous system and digestive system can both react at the same time, which is why nausea can come on quickly and feel intense.
Ondansetron may be used when:
The goal is comfort and stability. Controlling nausea early can help keep symptoms from escalating.
Nausea becomes more than a comfort issue when it starts to interfere with:
In these situations, ondansetron helps calm the stomach so other parts of detox can continue safely. It’s used as part of a broader medical plan and adjusted based on how symptoms change.
What Ondansetron (Zofran) Helps With — and What It Doesn’t
Helps With



Does Not Treat





Ondansetron is a prescription medication, but managing opioid or alcohol withdrawal at home can be dangerous and potentially life-threatening.
Ongoing vomiting can increase the risk of serious problems, including heart rhythm issues, seizures (especially with alcohol withdrawal), choking, blood pressure changes, confusion, and worsening withdrawal symptoms. Vomiting can also prevent other important medications from working when they’re needed most.
In medical detox, these risks are monitored closely and addressed right away. At home, symptoms can escalate quickly without warning.
Ondansetron is used to help with nausea and vomiting only. It does not treat withdrawal itself or the medical risks that can come with opioid or alcohol detox.
Ondansetron does not:
During medical detox, other medications are used to manage these symptoms and risks. For example, buprenorphine may be used for opioid withdrawal and cravings, and benzodiazepines are commonly used during alcohol detox to reduce seizure risk.
These medications work on different systems in the body. Ondansetron’s role is comfort — helping control vomiting so the body can better tolerate detox while other treatments address safety and withdrawal symptoms.
Ondansetron is commonly used in hospitals and medical detox settings and is generally well tolerated. When it’s used during opioid or alcohol detox, medical staff monitor symptoms and adjust care as needed.
Even as a comfort medication, there are a few safety points that matter during withdrawal.
Some people may experience mild side effects, including:
These side effects are usually manageable and often improve as nausea settles and the body stabilizes.
In some cases, ondansetron can affect heart rhythm. This risk is higher during detox because withdrawal, vomiting, and poor intake can affect the body’s balance.
Medical teams watch for:
Risk is higher for people with known heart rhythm conditions or low potassium or magnesium levels. This is why vitals and overall stability are monitored during detox.
Allergic reactions are uncommon, but staff should be notified right away if there is:
If nausea or vomiting continues, it doesn’t mean detox isn’t working. Withdrawal symptoms can change as the body adjusts. In medical detox, ongoing nausea signals the care team to reassess. Medications, fluids, or other parts of the plan may be adjusted to better support the body.
Withdrawal can affect the entire body, not just the stomach. While nausea and vomiting are common, there are times when withdrawal symptoms signal a need for medical care to prevent serious complications.
Medical detox is recommended when symptoms begin to affect safety, stability, or the ability to function.
Withdrawal should be medically managed when any of the following are present:
These signs mean the body is under more stress than it can safely manage on its own.
Withdrawal is unpredictable, especially in the first few days. Symptoms can escalate quickly and affect the heart, brain, and nervous system. In alcohol withdrawal, the risk of seizures or delirium can be life-threatening. In opioid withdrawal, severe symptoms can lead to dangerous complications, relapse risk, or medical emergencies.
In medical detox, symptoms are monitored closely. Medications, fluids, and supportive care can be adjusted in real time to keep the body stable and reduce risk.
Needing medical care during withdrawal does not mean someone is weak or that treatment is failing. It means the body needs help through a stressful and potentially dangerous process. Getting medical support early can prevent emergencies and make detox safer and more manageable.
Withdrawal symptoms can change quickly. If nausea, vomiting, or other symptoms feel hard to manage, medical detox can help keep things safer.
If symptoms are active or getting worse, speaking with a medical detox professional sooner can help prevent emergencies. Admissions teams can explain options and help you decide the safest next step.
Calls are confidential, available 24/7, and there’s no obligation to commit.
Get answers about your cost / coverage now.
Your information will be kept private
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!