Dorchester Addiction and Mental Health Treatment Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
In 2024, Boston recorded a 38% drop in opioid-related deaths—its lowest level since 2015. Yet neighborhoods like Dorchester continue to face higher risks than other parts of the city, reflecting the concentration of the crisis in areas near Mass and Cass, Roxbury, and the South End.
At the same time, Dorchester residents benefit from Boston’s broad treatment network, community-based recovery supports, and the city’s robust public health response, which has expanded outreach and treatment placements in recent years.
This guide outlines how to access addiction, mental health, and recovery services in Dorchester, helping residents navigate Boston’s comprehensive but complex system of care.
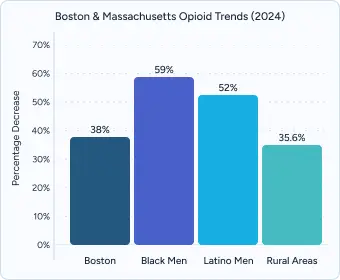
Boston saw a 38% decline in opioid-related overdose deaths in 2024, marking the lowest level since 2015 and the largest one-year decrease in nearly a decade. Black men experienced a 59% decrease and Latino men a 52% decrease from 2023, reflecting targeted outreach success. However, statewide figures show rural areas continue to face the highest overdose rates at 35.6 per 100,000 residents.
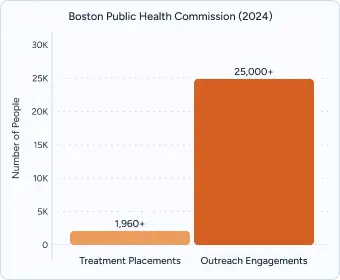
The Boston Public Health Commission placed more than 1,960 people into treatment in 2024. At the same time, formal treatment admissions declined, while outreach and harm-reduction teams expanded, engaging residents over 2,500 times annually through naloxone distribution and mobile crisis response.
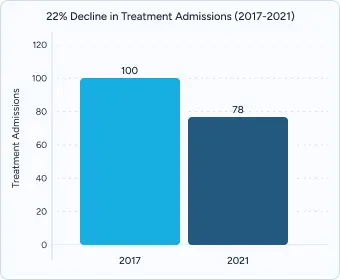
Despite city investments, treatment admissions among Boston residents fell 22% over a four-year period. Dorchester remains disproportionately affected by these gaps, with residents more likely to rely on emergency and street-level interventions rather than sustained treatment programs.
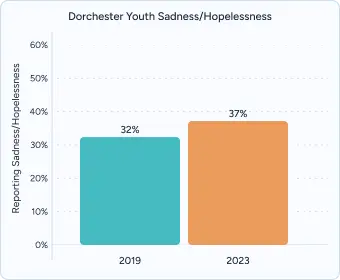
According to state youth surveys, nearly half of Dorchester adolescents report experiencing persistent feelings of sadness or hopelessness—up from 32% in 2019. Rates are particularly high among LGBTQ+ youth, Black and Latino students, and those from low-income families. Less than half of those reporting symptoms receive adequate support.

Crisis and urgent care access
Boston Medical Center’s Community Behavioral Health Center serves as a hub for urgent mental health and addiction treatment, offering walk-in and same-day care. The Boston Emergency Services Team (BEST) provides 24/7 mobile crisis response across all neighborhoods, including Dorchester, with adult and youth crisis stabilization units available.
Mobile crisis intervention
The BEST team distributes over 23,000+ naloxone kits annually, while also providing mobile evaluations, psychiatric care, and short-term stabilization. Residents can reach live clinicians anytime at 1-800-981-HELP.
Transportation access
Dorchester is connected to Boston’s treatment network through MBTA Red Line stations and multiple bus routes. The RIDE paratransit service also supports residents with disabilities, ensuring access to treatment hubs across the city.
MassHealth coverage
MassHealth covers 100% of treatment costs for eligible residents, including detox, residential, outpatient therapy, and FDA-approved medications like buprenorphine and methadone. As of 2025, there are no copayments for substance use treatment.
State-funded assistance
The Massachusetts Bureau of Substance Addiction Services provides financial support for those not eligible for MassHealth, up to 200% of the federal poverty level. Applications can be made online or through Department of Public Health regional offices.
City-level resources
Boston’s Access to Recovery and Wellness program offers wraparound funding and navigation services for uninsured residents. Call 311 or visit boston.gov/recovery-services for placement assistance, public treatment slots, and transportation support.
For those seeking private care without long wait times, several Massachusetts facilities—including options serving Dorchester—offer direct admission with insurance verification. These programs provide comprehensive assessment, medical detox, evidence-based therapies (Cognitive Behavioral Therapy (CBT), Dialectal Behavioral Therapy (DBT), Eye Movement Desensitization and Reprocessing (EMDR), and holistic approaches such as Yoga, Reiki, and Art Therapy.
Private programs often provide advantages such as:
The Haven Detox – New England serves the Dorchester area from its Worcester location. The center combines evidence-based therapies with holistic care, offering high staff-to-client ratios and personalized medication selection using GeneSight testing. Amenities include a professional chef, fitness facilities, recreational activities, and private spaces designed for healing.
The program specializes in dual diagnosis care, accepts most insurance plans including MassHealth, and offers transportation support across Massachusetts and nearby regions.
Mental health programs are available throughout Dorchester, with specialized services tailored to its diverse communities.
In the Lower Mills and Cedar Grove areas, families have access to counseling and mobile therapy services designed to meet cultural needs. Many programs focus on Latino communities, offering Spanish-language support and wraparound family services that extend care beyond the individual.
Uphams Corner and Columbia Point provide a range of supports including peer-led circles, faith-based counseling partnerships, and trauma-focused treatment. These services are particularly valuable for African American and Caribbean residents who may benefit from care rooted in cultural understanding and community connection.
In Fields Corner and Savin Hill, community health centers and Boston Medical Center affiliates deliver bilingual care for Vietnamese, Haitian, and African immigrant populations. These programs emphasize accessibility and culturally competent treatment, ensuring that diverse Dorchester neighborhoods can connect with resources that reflect their backgrounds and experiences.
The Metro Boston Recovery Learning Community provides peer-to-peer services, advocacy, and career coaching to help individuals in recovery build confidence and independence.
Codman Square Health Center Peer Support offers substance use outreach, harm reduction resources, and culturally responsive programming designed for the Dorchester community.
The Boston Medical Center Recovery Learning Community employs peer specialists who support crisis evaluations, provide advocacy, and assist with follow-up care to strengthen recovery outcomes.
MASH-certified recovery homes in Dorchester meet state and national standards, offering structured housing with 24/7 peer support, secure entry, and consistent programming.
Most homes require weekly meetings, regular sobriety monitoring, and active community participation to help residents stay accountable in their recovery journey.
Boston AA Central Service coordinates more than 2,200+ meetings each week across Eastern Massachusetts, including groups based in Dorchester neighborhoods.
Spanish-speaking AA groups hold regular meetings in Dorchester churches and community centers, providing culturally relevant recovery support for Latino residents.
Young adult recovery groups in Dorchester offer hybrid in-person and virtual meetings, pairing younger participants with peer sponsors and a supportive community.
Effective treatment in Dorchester should address both addiction and mental health conditions together, since co-occurring disorders are common. Many residents face challenges such as trauma, depression, or anxiety alongside substance use, making integrated care essential for long-term recovery.
Dorchester’s neighborhoods are among the most diverse in Boston, and programs that recognize cultural needs can better engage residents in care. Access to bilingual providers, LGBTQ+-affirming services, and faith-based or culturally rooted programming is especially important for Latino, Haitian, Vietnamese, and African immigrant communities. Holistic therapies also play a valuable role in recovery by addressing stress, building resilience, and supporting overall well-being.
Recovery does not end when treatment does. Strong programs in Dorchester begin planning for aftercare early, connecting clients to outpatient services, peer-led recovery groups, and transitional housing. These warm handoffs make it easier to stay engaged in care and avoid relapse.
Professional treatment provides a level of medical supervision that cannot be matched outside a clinical setting. Licensed staff monitor patients around the clock, reducing withdrawal risks and ensuring immediate care in emergencies.
Every person’s recovery path is different. Professional programs use comprehensive assessments to design customized care plans, backed by experienced clinicians and low client-to-staff ratios for focused support.
Reputable facilities follow strict national guidelines and collaborate with outside providers to maintain safety and effectiveness. Accreditation demonstrates a commitment to quality and accountability.
Healing happens best in environments designed for comfort, privacy, and overall well-being. High-quality amenities reduce stress and make it easier to focus fully on recovery.
In a crisis, waiting for treatment can be dangerous. Professional programs that offer immediate admission help people stabilize quickly, reduce overdose risk, and begin recovery without unnecessary delays.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Recovery doesn’t have to wait. Professional support is available 24/7 to help Dorchester residents begin treatment quickly.
Insurance and coverage support
Financial advocates review benefits, provide cost estimates, and assist with prior authorizations so patients can focus on care.
Streamlined admissions
Same-day psychiatric evaluations and next-day placements are available when beds are open, with staff guiding every step of the process.
Most programs in Boston, including Dorchester, schedule an intake within 48 hours, though wait times can be longer if demand is high. Some private facilities may be able to offer same-day assessments or quicker placement when beds are available.
Yes. MassHealth covers individual and group therapy at no cost, including outpatient counseling, psychiatric visits, and family therapy. Most Dorchester providers accept MassHealth, and coverage can be confirmed by calling 1-800-841-2900. Private programs typically complete insurance verification more quickly, often within 24 hours.
Yes. Dorchester hosts Spanish-language AA/NA groups, Haitian Creole recovery circles, and bilingual facilitators through Codman Square and community centers. Vietnamese and Portuguese speakers can often access interpreter services through mobile crisis teams or the Massachusetts Behavioral Health Help Line (833-773-2445).
Yes. Community health centers like DotHouse and Codman Square offer sliding-scale fees, and Boston’s Recovery Services program connects residents with publicly funded treatment slots. Some private providers also offer financial counseling and flexible payment options to make care more accessible.
Yes. MBTA’s The RIDE paratransit service supports individuals with disabilities, while some programs offer bus vouchers or shuttle services. Mobile crisis teams may also provide direct transport to stabilization units. Private programs sometimes help coordinate transportation to ensure patients can enter care quickly.
Crisis hotlines operate 24/7. Call BEST at 1-800-981-HELP for mobile crisis response in Boston, or 1-877-382-1609 for statewide crisis intervention. You can also dial 988 for suicide prevention.
Yes. Family peer specialists at Codman Square and Boston Medical Center provide coaching, and Al-Anon meetings are available throughout Dorchester. These services help families navigate next steps and plan interventions. Some private facilities also work directly with families to support admissions when a loved one is hesitant.
Codman Square offers Latino-focused counseling; DotHouse provides Haitian Creole-speaking staff; and Fields Corner programs support Vietnamese, African immigrant, and Caribbean families with bilingual care. Many also include faith-based counseling partnerships.
Yes. Dorchester has youth recovery groups for ages 18–30, with peer sponsors and support tailored to education or career stress. The Metro Boston Recovery Learning Community also provides young adult programming. Private providers sometimes run specialized tracks for young adults and students, with faster intake options when needed.
Boston Public Health Commission. New data show 38% decline in opioid-related deaths in Boston in 2024, following national trend. Published June 3, 2025. Accessed September 11, 2025. https://www.boston.gov/news/new-data-show-38-decline-opioid-related-deaths-boston-2024-following-national-trend
Boston Public Health Commission. Health of Boston 2023–2024: Substance Use and Disorders. Published April 1, 2024. Accessed September 11, 2025. https://www.boston.gov/sites/default/files/file/2024/06/HOB_SUD_2023_1Apr2024.pdf
City of Boston Public Health Commission. New data show 38% decline in opioid-related deaths in Boston in 2024, following national trend. Boston.gov. Published May 29, 2025. Accessed September 11, 2025. https://www.boston.gov/news/new-data-show-38-decline-opioid-related-deaths-boston-2024-following-national-trend
Massachusetts Department of Public Health. Opioid-related overdose deaths, all intents by city/town, 2010–2023. Accessed September 11, 2025. https://www.mass.gov/lists/current-overdose-data
MassHealth. Member copayments and deductibles. Updated January 2025. Accessed September 11, 2025. https://www.mass.gov/info-details/masshealth-copayment-information-for-members
Massachusetts General Court. Chapter 285 of the Acts of 2024: An Act Relative to Substance Use Disorder Treatment and Prevention. Approved December 2024. Accessed September 11, 2025. https://malegislature.gov/Laws/SessionLaws/Acts/2024/Chapter285
Boston Public Schools. Youth Risk Behavior Survey (YRBS) 2023 Results: Boston High Schools. Published 2023. Accessed September 11, 2025. https://www.bostonpublicschools.org/bps-departments/health-and-wellness/data-evaluation/youth-risk-behavior-survey/results-data-requests/boston-high-school-yrbs-results
Boston Public Health Commission. Health of Boston: Mental Health 2024. Published 2024. Accessed September 11, 2025.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!