
New Jersey Addiction and Mental Health Resources
When time is critical, accessing professional detox and psychiatric support can be lifesaving. New Jersey saw overdose deaths drop from 3,171 in 2022 to 2,816 in 2023—a decline of 11.2%—yet illicit fentanyl, implicated in over 80% of overdose fatalities, continues to drive the crisis. Only about 52% of adults with a mental illness received treatment last year, while 22% faced unmet needs due to provider shortages and insurance hurdles.
Private treatment centers offer rapid admission, 24/7 medical supervision for safer withdrawal, and integrated behavioral health services to address co-occurring disorders. Their evidence-based therapies and medication management ensure the most reliable path to stabilization and long-term recovery, even when state-funded programs are at full capacity.
Need Professional Treatment Today? The Haven Detox – New Jersey provides immediate access with medical supervision for safer, more comfortable withdrawal management and comprehensive mental health care.
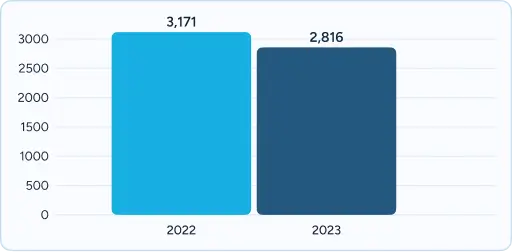
2,816 suspected overdose deaths in 2023, a decline from 3,171 in 2022 — averaging more than 7 lives lost per day.
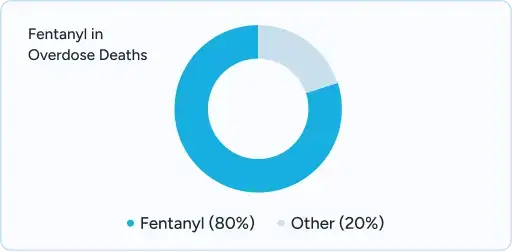
Fentanyl is involved in more than 80% of overdose deaths.
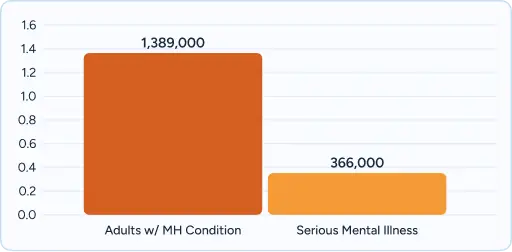
1,389,000 adults in New Jersey live with a mental health condition, including **366,000 with serious mental illness (SMI).
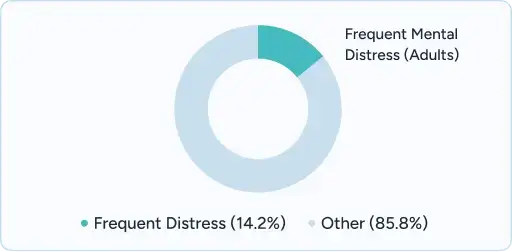
14.2% of NJ adults report frequent mental distress (14+ days/month).

ED visits with a mental health or substance use disorder diagnosis averaged 60.9 per 1,000 population statewide, but in vulnerable zip codes like Camden and Newark exceeded 500 per 1,000..

New Jersey ranks 22nd nationally for adult mental health care access
While treatment waitlists are discouraged by state policy, high demand and limited inpatient beds mean many residents still experience delays, especially in rural areas.
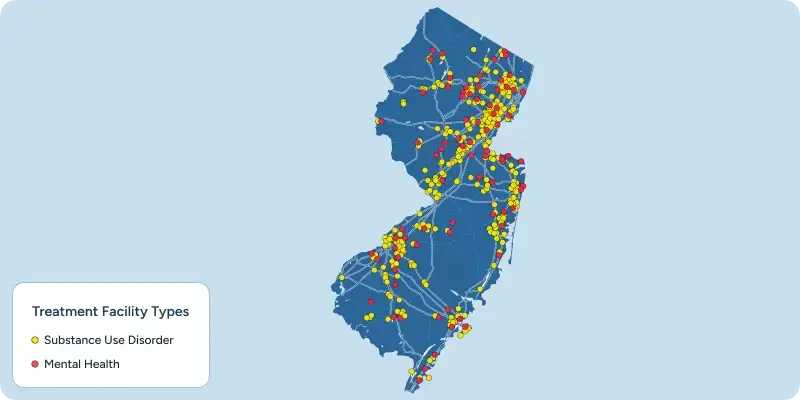
New Jersey plays a central role in the Mid-Atlantic behavioral health system, with treatment resources that serve both state residents and people across the Northeast corridor. Specialized facilities are spread across all 21 counties, with larger hubs in Newark, Jersey City, Trenton, and Atlantic City helping anchor access to care.
The state’s location and transportation network make treatment relatively accessible compared to many regions. Interstate highways (I-95, I-287, and the Garden State Parkway), NJ Transit rail lines, and Newark Liberty International Airport connect patients from neighboring states including New York, Pennsylvania, Delaware, and Connecticut. About 30% of residential treatment admissions in New Jersey come from out of state, reflecting both demand for services and gaps in access elsewhere.
New Jersey supports a wide treatment ecosystem, with more than 369 facilities ranging from medical detox centers to residential programs. At the same time, the state continues to face regional disparities: urban and northern counties often have more resources, while rural and southern areas report fewer specialty programs and longer wait times.
Treatment settings also vary. Urban programs often focus on outpatient and high-volume services, while coastal and rural programs may offer more residential or recovery-focused environments. Combined with New Jersey’s relatively strong insurance coverage mandates and mental health parity laws, these factors make the state a significant provider of addiction and mental health care — though access remains uneven depending on location and level of need.
New Jersey has a robust behavioral health system compared to many states, with dedicated psychiatric hospitals, detox facilities, and CCBHCs. But families still face barriers that delay or complicate access:
These challenges highlight why many families turn to professional treatment centers that offer integrated programs, streamlined access, and immediate admissions.

Accessing quality care shouldn’t mean navigating confusing insurance hurdles. In New Jersey, both NJ FamilyCare (Medicaid) and major private health insurers cover a wide range of behavioral health services. Below is an overview of what’s included and how our facilities work with these insurers to make treatment accessible, affordable, and effective.
NJ FamilyCare provides healthcare coverage for eligible New Jersey residents, including comprehensive behavioral health services.
As of January 2025, NJ FamilyCare began transitioning behavioral health services into managed care networks, making it easier for members to receive outpatient mental health and substance use disorder treatment directly through their plan. Our facilities participate with NJ FamilyCare managed care organizations (MCOs), so members can access high-quality, accredited treatment with reduced out-of-pocket costs.
Horizon Behavioral Health℠ provides members with access to therapy, psychiatric evaluations, medication management, substance use treatment, intensive outpatient programs (IOP), partial hospitalization, and residential care. Crisis intervention and telehealth options are also available.
Aetna covers a wide range of behavioral health services, including outpatient counseling, psychiatric care, substance use disorder treatment, and higher levels of care such as IOP, PHP, and residential programs.
UnitedHealthcare and Oxford offer mental health and addiction treatment coverage that includes outpatient counseling, medication-assisted treatment (MAT), IOP, and residential services when medically necessary.
Cigna Healthcare provides behavioral health benefits through the Cigna Behavioral Health network, covering outpatient therapy, medication management, substance use disorder care, IOP, and residential treatment.
Because Cigna relies on in-network, accredited providers, members can receive comprehensive services with lower out-of-pocket costs.
AmeriHealth provides PPO and HMO plans in New Jersey with behavioral health benefits that include outpatient therapy, psychiatric care, and substance use disorder treatment. Many plans also cover IOP, PHP, and residential care when clinically appropriate.
Horizon NJ Health serves NJ FamilyCare members and, beginning in January 2025, now manages outpatient behavioral health services directly through its network. Coverage includes outpatient counseling, psychiatric care, addiction treatment, and crisis support.
New Jersey offers a wide range of state-funded behavioral health services, including detox programs, outpatient clinics, and crisis stabilization. These services provide essential support, but families often encounter fragmented systems, waitlists, and uneven access across regions.
By contrast, professional treatment centers streamline the entire process. Families benefit from:
This difference can determine whether a family faces barriers and delays — or receives timely, coordinated treatment.
| Care Coordination | |
| Admission Times | |
| Insurance Navigation | |
| Emergency Department Impact | |
| Regional Reach | |
| Specialized Programs |
| Care Coordination | |
| Admission Times | |
| Insurance Navigation | |
| Emergency Department Impact | |
| Regional Reach | |
| Specialized Programs |
DMHAS funds peer-led recovery centers that provide:
New Jersey residents can find trusted local information on addiction treatment, recovery services, and mental health support through The Haven Detox’s city-based resource guides. Each guide highlights regional programs, behavioral health systems, and community resources tailored to local needs.
New Jersey’s state-funded programs form the foundation of access, but professional centers can deliver the timeliness, expertise, and environment families often need in urgent crises.
Verify benefits and understand your treatment options
Compare programs, read reviews, and make informed decisions
If you or a loved one is experiencing a mental health or substance use crisis, help is available right now:
Yes. Coverage includes detox, residential, outpatient, MAT, and crisis stabilization. Members with a Serious Mental Illness (SMI) designation qualify for expanded services like case management and housing【NJ FamilyCare】.
Professional residential programs typically run 30–90 days. State-funded programs often limit stays to 2–4 weeks for stabilization.
Most are concentrated in northern and central NJ (Newark, New Brunswick, Trenton). South Jersey has fewer inpatient options.
While New Jersey has a dense behavioral health system, care is often fragmented across different providers, insurance networks, and county programs. Families may face referrals, paperwork, or insurance approvals that delay access. Professional treatment centers can simplify this process by offering integrated care and direct admissions, avoiding unnecessary ER visits or wait times.
Yes. Programs exist for veterans, LGBTQ+ residents, immigrant families, and faith-based communities. NAMI NJ also runs culturally tailored affiliates and support groups.
NJ offers 24/7 crisis hotlines and mobile crisis teams statewide. Professional facilities may also provide same-day admission, avoiding delays.
Options include alumni programs, DMHAS-funded peer recovery centers, and NAMI NJ peer and family support groups.
Yes. Homes must register with DMHAS, and some pursue voluntary certification for quality oversight.
Be cautious of facilities that promise a cure, lack licensing/accreditation, provide no 24/7 medical coverage, or discourage family involvement.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!