
Florida Addiction and Mental Health Treatment Resource Guide
Finding addiction or mental health treatment in Florida can feel overwhelming, especially given the state’s urgent challenges. Florida ranks #1 in the nation for adults living with mental illness, with nearly 3 million people—17.5% of the adult population—affected. Substance use disorders are just as alarming: in 2023, Florida recorded 7,220 fatal overdoses, while fentanyl alone was linked to 5,302 deaths in 2020.
Yet, despite the scale of need, access to effective care remains limited. Only 28% of Medicaid enrollees diagnosed with opioid use disorder receive evidence-based medication-assisted treatment in Florida, leaving thousands without life-saving support. Even more concerning, 74.6% of people who need substance use treatment never receive it, highlighting a massive gap in care.
These realities underscore the urgent importance of seeking professional addiction treatment in Florida or comprehensive mental health services. With expert medical intervention, individuals and families can find stability, healing, and hope at The Haven Detox – Florida — replacing these sobering statistics with real stories of recovery and resilience.
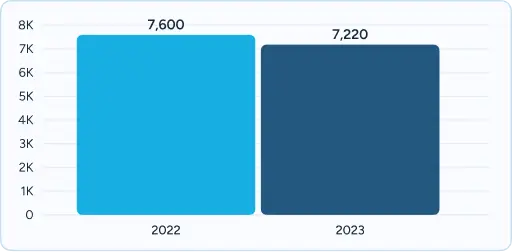
Fatal Overdoses: 7,220 in 2023 (-5.0% vs 7,600 in 2022)
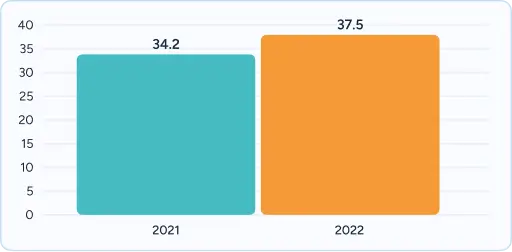
Age-Adjusted Rate: 37.5 deaths per 100,000 in 2022 (18th nationally; +9.6% vs 34.2 in 2021)
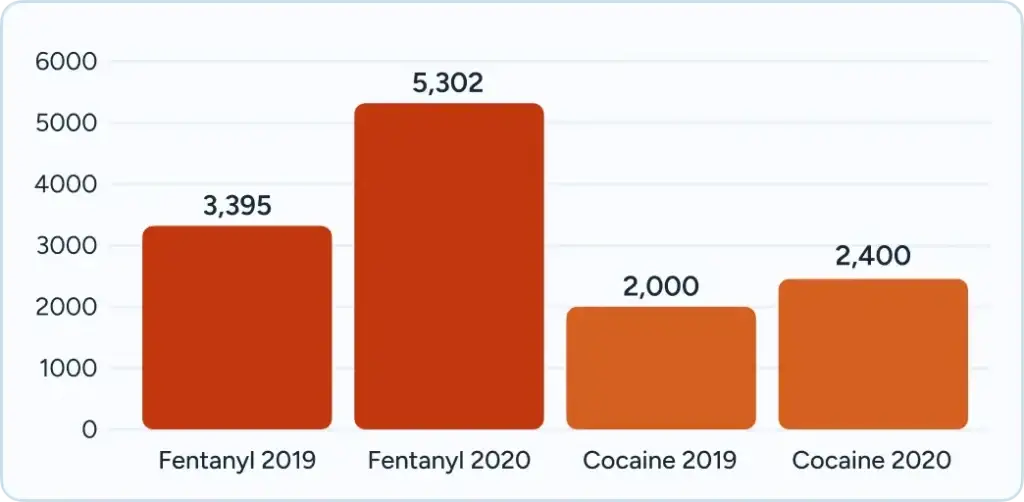
Fentanyl Deaths: 5,302 in 2020 (+56% vs 3,395 in 2019*), followed by cocaine at 2,400 in 2020 (+20% vs 2,000 in 2019*)
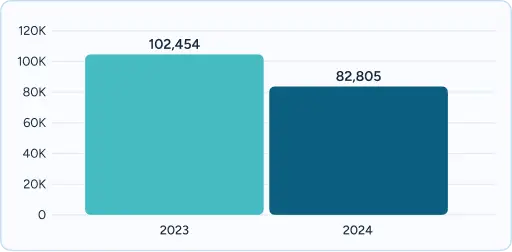
EMS Overdose Responses: 82,805 in 2024 (-19% vs 102,454 in 2023)
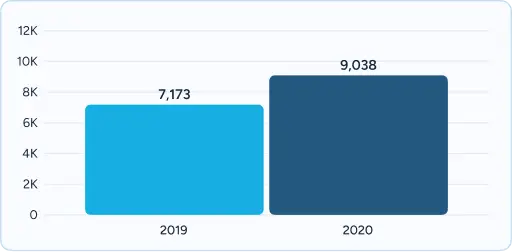
Over 9,038 Floridians died with prescription drugs detected in their system in 2020, marking a 26% increase from the previous year
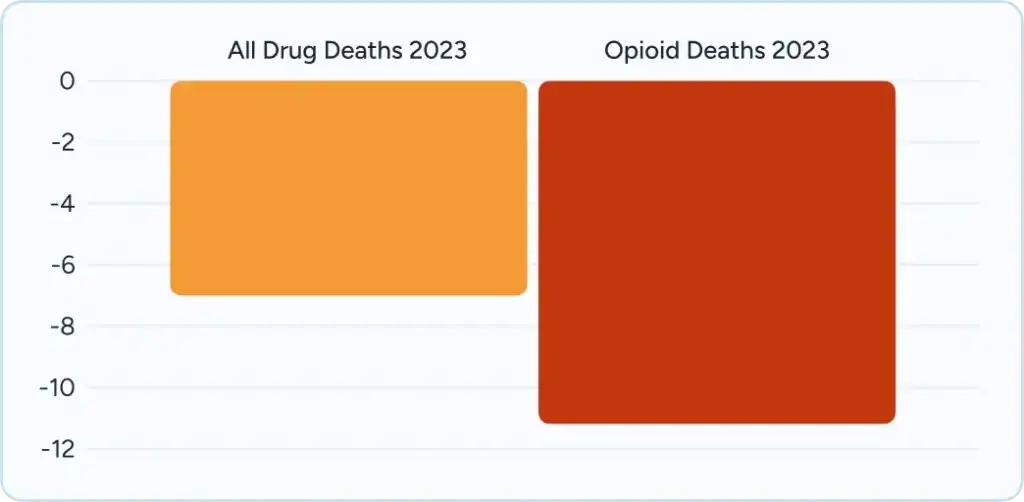
Drug overdose deaths decreased by 7% in 2023 compared to 2022⁵, though opioid-related deaths decreased by 11%
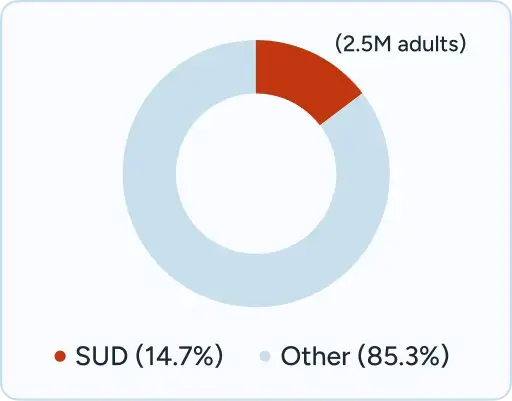
14.73% of people age 12 and older have a substance use disorder⁴, affecting approximately 2.5 million adults
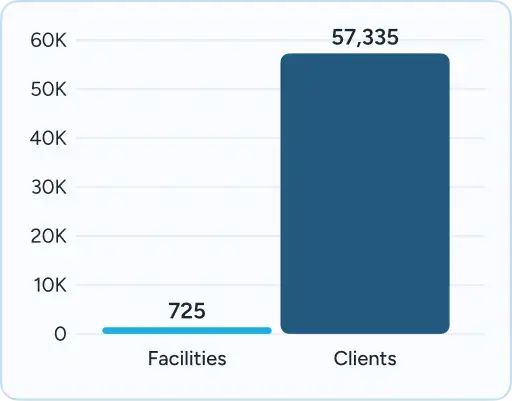
725 substance abuse treatment facilities operate statewide, serving 57,335 clients as of March 2019
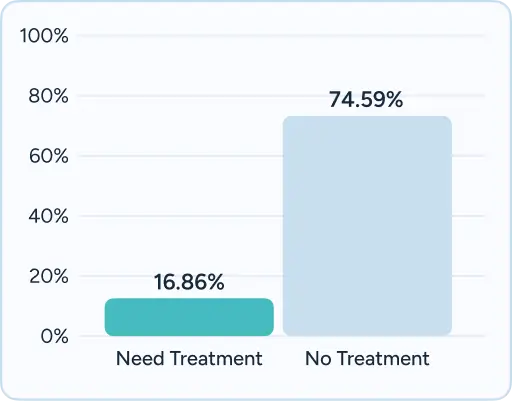
16.86% of people classified as needing substance use treatment, but 74.59% of those needing treatment do not receive it
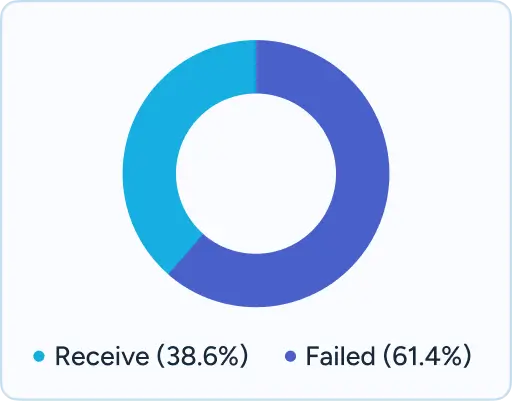
61.4% of adults with mental illness failed to receive treatment in 2021
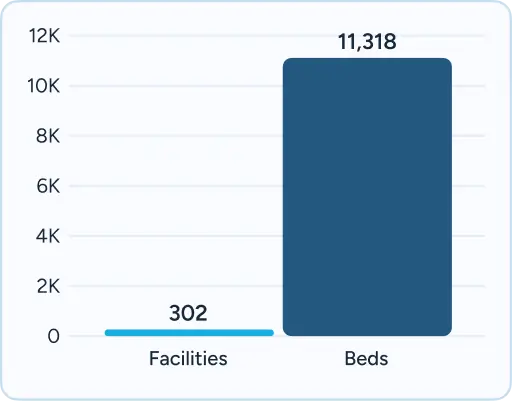
Florida has 302 facilities serving adults with 11,318 beds total for various levels of psychiatric care

| Waiting Times | |
| Provider Availability | |
| Funding Constraints | |
| Administrative Burden | |
| Quality and Standards |
|
| Service Scope | |
| Withdrawal & Dual Diagnosis | |
| Therapy Approach |
| Waiting Times | |
| Provider Availability | |
| Funding Constraints | |
| Administrative Burden |
|
| Quality and Standards |
|
| Service Scope | |
| Withdrawal & Dual Diagnosis | |
| Therapy Approach |
Florida has emerged as a premier destination for addiction and mental health treatment, serving not only its residents but also individuals from across the Southeast and beyond. The state’s strategic location and comprehensive infrastructure make it highly accessible to those seeking recovery services. Major cities including Miami, Tampa, Orlando, Jacksonville, and Fort Lauderdale host numerous world-class treatment facilities, offering everything from medical detoxification to long-term residential care.
The state’s extensive highway system and multiple international airports provide exceptional accessibility for out-of-state patients and their families. Interstate 95 connects Florida to the entire Eastern seaboard, while I-75 and I-10 provide direct access from the Midwest and Western states. This transportation infrastructure has contributed to Florida becoming a regional treatment hub, with a substantial amount of private treatment facility admissions coming from out-of-state residents seeking specialized care in the state’s favorable climate and diverse treatment options. NBC News reported in 2017 that an industry group tally found 75% of young people in treatment in Florida are from out of state.
Florida’s treatment ecosystem spans from specialized dual diagnosis programs in South Florida to comprehensive family therapy centers in Central Florida, offering unprecedented variety in treatment approaches. The state’s year-round temperate climate supports outdoor therapy programs, adventure-based treatment modalities, and extended family programming that draws patients from colder climates. Neighboring states including Georgia, Alabama, South Carolina, North Carolina, and Tennessee regularly refer patients to Florida facilities, recognizing the state’s expertise in complex cases and innovative treatment approaches.

Navigating insurance coverage for behavioral health services can be extraordinarily complex, with varying benefits, prior authorization requirements, and network restrictions that often confuse patients and families during already difficult times. Professional treatment centers recognize these challenges and employ specialized insurance verification teams who work directly with insurance companies to verify benefits, obtain prior authorizations, and explain coverage details in understandable terms.
Residents across Florida can access localized addiction and mental health resources designed to connect individuals and families with care in their communities. Each city guide provides detailed information about local treatment programs, recovery services, and behavioral health supports.
While Florida offers excellent public resources, professional treatment facilities provide distinct advantages when immediate care is needed:
Recovery is not only possible but achievable with the right professional support and evidence-based treatment approaches. Professional treatment centers throughout Florida offer genuine hope for long-term recovery, providing the medical expertise, therapeutic interventions, and comprehensive support systems necessary for lasting change. With Florida ranking first nationally in adults experiencing mental illness and recording over 7,000 overdose deaths in 202315, the need for immediate, professional intervention has never been more critical.
Verify benefits and understand your treatment options
Compare programs, read reviews, and make informed decisions
If you or a loved one is experiencing a mental health or substance use crisis, help is available right now:
Private treatment facilities typically offer same-day or next-day admissions with 24/7 intake processes, while state-funded facilities may have waiting periods ranging from several days to weeks depending on the level of care needed. Emergency psychiatric services and crisis stabilization are available immediately through hospital emergency departments and mobile crisis teams responding within 60 minutes.
Florida Medicaid covers a comprehensive range of behavioral health services including inpatient and outpatient treatment, therapy, medication management, and crisis services. Many private facilities accept Medicaid, though coverage and authorization requirements vary by provider and specific treatment services requested.
Out-of-state residents can access treatment in Florida, with an estimated 30-40% of private facility admissions coming from other states. Interstate insurance coverage often applies, though verification of benefits is essential. Florida’s accessibility via major highways and international airports makes it a regional treatment destination.
Florida emphasizes integrated dual diagnosis treatment approaches where addiction and mental health conditions are treated simultaneously by coordinated clinical teams. Florida Assertive Community Treatment (FACT) teams provide comprehensive community-based services, while residential facilities offer specialized dual diagnosis programming.
Florida’s Baker Act allows involuntary psychiatric examination for up to 72 hours when someone poses a danger to themselves or others due to mental illness. The Marchman Act provides similar provisions for substance abuse, though recent legislation has streamlined these processes with more flexible court-ordered treatment options.
Professional treatment centers typically offer alumni support services, readmission policies, and continuing care programs. Many facilities provide free aftercare support, alumni meetings, and crisis intervention for graduates. Florida’s peer recovery specialist network offers ongoing support, while Mobile Response Teams provide 24/7 crisis intervention.
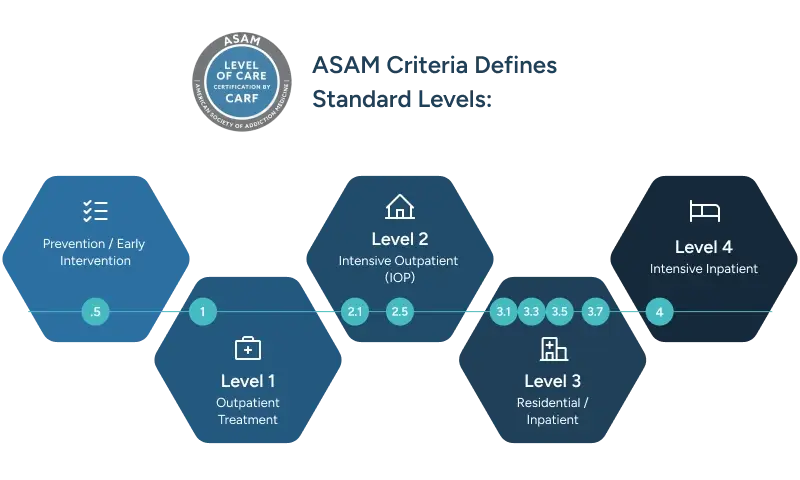
Medical detoxification typically lasts 3-7 days, residential treatment ranges from 30-90 days depending on clinical need, and outpatient services can continue for months or years as clinically appropriate. Florida’s treatment system emphasizes individualized care planning with length of stay determined by patient progress and clinical recommendations.
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!