Plymouth Addiction Treatment & Mental Health Resources Guide
Dr. Rostislav Ignatov, MD
Chief Medical Officer
Plymouth, MA faces an evolving addiction and behavioral health challenge. In 2023, the town recorded 18 confirmed opioid-related overdose deaths, while Plymouth County overall saw a 14% increase in overdose deaths in 2022—one of the largest year-over-year rises in the state. Despite these troubling trends, the region maintains a network of supports that includes outpatient behavioral health care, statewide Community Behavioral Health Centers (CBHCs), and county-level providers serving the South Shore and Cape Cod.
Plymouth residents can access both public and private treatment pathways depending on their needs. The Plymouth Community Behavioral Health Center (CBHC) is part of Massachusetts’ statewide CBHC. For those seeking private care without long wait times, The Haven Detox – New England in Worcester offers medical detox, residential treatment, and integrated dual-diagnosis care in a comfortable, resort-style setting with wellness amenities. Together, these options illustrate the spectrum of care available to Plymouth residents, from publicly funded safety-net services to immediate private admission for those ready to begin recovery.
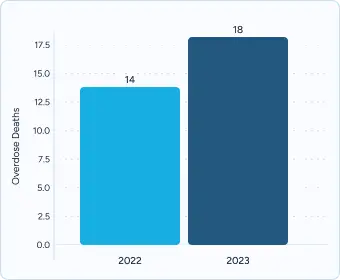
The town of Plymouth recorded 18 confirmed opioid-related overdose deaths in 2023. By comparison, Plymouth had 14 overdose deaths in 2022, reflecting a year-over-year increase of nearly 29%. While these numbers are smaller than in larger cities, the upward trend underscores the growing pressure on local treatment systems.
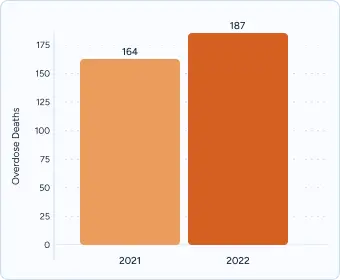
Plymouth County as a whole experienced a 14% rise in opioid-related overdose deaths between 2021 and 2022, one of the sharpest increases statewide. In 2022, the county recorded 187 overdose deaths, up from 164 in 2021, outpacing the statewide average and signaling a regional crisis.
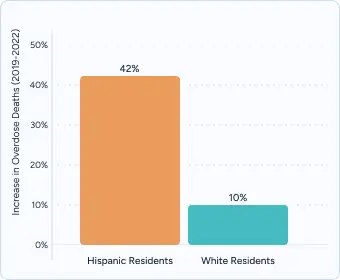
Statewide data show opioid-related overdose deaths among Hispanic residents rose by 42% between 2019 and 2022, compared to smaller increases among White residents. While Plymouth-specific breakdowns are limited, county and state data suggest Hispanic communities in Plymouth and across the South Shore have been disproportionately impacted. This disparity underscores the need for culturally responsive outreach, bilingual providers, and expanded access to treatment tailored to diverse populations.

According to the Massachusetts Youth Health Survey (MYHS), 28% of surveyed students in grades 6-12 reported prolonged sadness or hopelessness in 2023. This statewide figure provides a useful benchmark for comparing youth distress levels in smaller towns like Plymouth, especially when local services may not match urban capacity.
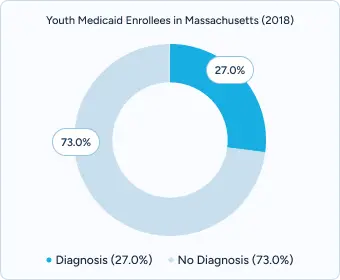
An Urban Institute analysis found that in Massachusetts, approximately 27% of adolescent Medicaid enrollees had either a mental health or substance use diagnosis in 2018, highlighting that behavioral health needs are widespread among lower-income youth. This suggests that even youth who aren’t captured by school survey data may have significant unmet clinical needs, particularly in less-served areas.

Plymouth County Outreach serves as a centralized access point for treatment information and referrals. The program includes mobile crisis intervention and community naloxone distribution, distributing over 465 boxes of naloxone in 2021. The Plymouth County Drug Abuse Task Force provides 24/7 crisis intervention, covering Plymouth, Carver, Kingston, and surrounding areas. With locations at drop-in centers in Plymouth and East Bridgewater, it offers peer support, resource coordination, and a growing network of community partnerships.
Transportation accessibility through the Plymouth Area Link connects all neighborhoods to Plymouth drug rehab programs and mental health facilities. The GATRA transit system provides access to High Point Treatment Center, while specialized transportation through Taking People Places connects downtown to areas like Manomet and Plymouth Beach. The Massachusetts Bay Transportation Authority offers specialized transportation for individuals with disabilities seeking treatment services.
Covers 100% of treatment costs for qualified residents, including medical detox, residential treatment, outpatient therapy, and approved medications like buprenorphine and naltrexone. As of 2024, copayments have been eliminated for behavioral health services, extending coverage to residents up to 138% of federal poverty level.
Residents can enroll via the Massachusetts Health Connector online portal or by calling 1-800-841-2900, with applications available in English, Spanish, Portuguese, and other languages
Apply through the Massachusetts Department of Public Health regional offices or online, with support materials available in multiple languages including interpretation services.
Visit the Plymouth County website at plymouth-ma.gov or call 508-830-4357 to find public treatment slots and support resources across community agencies.
Private facilities eliminate wait times through free insurance verification, comprehensive assessment within 24 hours, medical detox availability, and evidence-based therapies including EMDR, family systems therapy, and mindfulness-based relapse prevention.
Insurance processing typically completes within 48 hours with same-day admission capabilities when clinically appropriate and medically safe.
The Haven Detox – New England in Worcester is a local professional treatment center that combines traditional therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) with holistic approaches, including Reiki, art therapy, and yoga, plus cutting-edge GeneSight genetic testing to personalize medication selection.
With one of the highest staff-to-client ratios in Massachusetts, the Worcester location provides both medical detox and residential treatment in a comfortable, resort-like environment for residents of Plymouth County.
Plymouth residents have access to a wide range of supports, including depression treatment, anxiety care, dual-diagnosis assistance, and trauma-informed therapy. Beth Israel Deaconess Hospital–Plymouth extends integrated behavioral health services through mobile therapy units and flexible options for those facing transportation or financial barriers.
Neighborhood programs make mental health care accessible across Downtown, Manomet, and South Plymouth. Downtown Plymouth includes counseling through local providers and hospital outreach, while South Shore communities benefit from peer-led support circles, faith-based counseling partnerships, and other local initiatives designed to foster resilience and well-being.
Free, community-based recovery programs provide social connection, peer support, and practical assistance:
Plymouth Recovery Center in Downtown Plymouth (5 Main Street Extension) offers free peer-led recovery support, specialized support groups for various stages of recovery, sober social events, and computer access for job readiness activities.
Gandara Center Recovery Support in Plymouth provides peer facilitated support groups, relapse prevention and tobacco cessation programs, and advocacy and recovery coaching services with flexible evening hours and weekend programming.
South Shore Community Services in nearby Brockton (15 Main Street) offers culturally responsive groups for diverse populations, transit accessibility via GATRA bus routes, and social media community engagement through active Facebook presence.
MASH-certified sober living homes provide structured transitional housing with comprehensive support services.
Massachusetts Alliance for Sober Housing (MASH) certification ensures quality standards and eligibility for state agency referrals, with the complete directory available at mashsoberhousing.org.
The Hillside Men’s Sober House holds MASH Level 2 certification and provides 24-hour peer support, keyless entry system, Wi‑Fi and laundry facilities, and structured programming. Residents participate in weekly house meetings, attend outside recovery meetings, maintain sobriety through regular screenings, and contribute to household responsibilities.
The Nook Men’s Recovery Residence maintains MASH accreditation and offers secure entry systems, community kitchen access, shared living spaces, and transportation assistance. House rules include weekly drug/alcohol screenings, meeting attendance requirements, structured curfews, and participation in recovery programming.
Plymouth County recovery meetings provide peer support through established mutual-aid programs.
Plymouth County Outreach coordinates over 150 meetings per week through partnerships with mobile apps and daily schedule updates, with the complete directory available at plymouthcountyoutreach.org and 24/7 helpline support at 508-261-5488.
Alcoholics Anonymous Plymouth serves English-speaking residents through multiple daily meetings at locations including Church of Pilgrimage, St. Mary’s Parish Hall, and Zion Lutheran Church, offering discussion, speaker, and step-study formats with wheelchair accessibility.
Narcotics Anonymous South Shore provides specialized meetings for substance users through the New England Region network, with meetings at First Baptist Church, Church of the Good Shepherd, and Plymouth Recovery Center featuring open discussion, literature study, and closed gender-specific options.
Comprehensive assessment should begin every treatment journey, evaluating both substance use and mental health needs. In Massachusetts, more than 50% of individuals with a substance use disorder also have a co-occurring mental health condition, underscoring the importance of integrated dual-diagnosis care. The most effective programs also involve family members in the assessment process, helping to build stronger support systems that improve long-term outcomes.
Evidence-based therapies form the backbone of effective treatment. Approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Trauma-Focused Therapy are proven to reduce relapse risk and improve mental health stability. Research shows that participation in evidence-based therapies can reduce the likelihood of relapse by up to one-third, highlighting their role in sustainable recovery.
Culturally responsive care ensures that treatment reflects the backgrounds and values of those it serves. In Plymouth County, where nearly 6% of residents identify as Hispanic or Latino and 2% as Cape Verdean or Portuguese-speaking, providers increasingly offer bilingual clinicians, LGBTQ+-affirming groups, and faith-compatible programming. These approaches help bridge cultural gaps and engage communities that historically face higher barriers to treatment.
Lasting recovery depends on more than the first 30 days of treatment. National research shows that people who remain engaged in structured care for 90 days or longer achieve significantly better outcomes. That’s why discharge planning begins during active treatment—not after. Strong programs connect clients with outpatient therapy, peer-led recovery groups, and sober living environments before they leave residential care. These warm handoffs between providers reduce relapse risk and help individuals transition smoothly into the next stage of recovery.
Family participation is another cornerstone of effective continuing care. Studies show that involving family in therapy can reduce relapse risk by up to 25%, while also improving communication and accountability. Many Plymouth-area programs now offer family therapy services in multiple languages, including Spanish and Portuguese, so that immigrant and bilingual households can access support that fits their needs.
Together, these continuing care supports create a safety net around recovery. They recognize that addiction is not a short-term issue, but a long-term health condition that requires ongoing structure, accountability, and community engagement.
Professional treatment offers more than just a safe environment—it provides medical expertise, personalized planning, and long-term supports that community-based care alone cannot match.
Effective treatment requires more than detox and counseling—it demands a complete system of supports. Trauma-informed care is foundational, with therapies such as EMDR and somatic experiencing helping patients process unresolved pain that drives substance use.
Programs also extend recovery beyond discharge through alumni networks that maintain accountability and peer connection. Graduates often join mentorship programs, quarterly reunions, or digital support platforms that keep them tied into a recovery community long after leaving inpatient care.
Case management and benefits navigation services provide another vital layer, helping clients secure insurance coverage, stable housing, and employment resources. By reducing financial and logistical stress, case management has been shown to increase treatment retention and long-term recovery success.
Finally, modern treatment recognizes the importance of holistic healing. Nutrition support, fitness activities, mindfulness training, and expressive therapies like art or music help clients restore balance in both body and mind. These offerings not only make treatment more comfortable but also equip patients with lifelong coping tools to sustain recovery.
Professional treatment represents an investment in recovery success, offering immediate access, personalized care, and comprehensive services designed to address the complex nature of addiction and mental health conditions.
Begin your recovery journey with comprehensive evaluation and immediate access to life-changing treatment.
Insurance and Benefits Verification provides coverage estimates within 24–48 hours and financial assistance applications for uninsured residents, including Medicaid enrollment support and Health Safety Net program coordination.
Assessment and Intake Services offer same-day comprehensive evaluations and next-day placement in appropriate level of care, featuring streamlined admission procedures that minimize administrative delays and support readiness for recovery.
Most Plymouth programs schedule an intake within 48 hours, but demand can extend wait times. Private facilities like The Haven Detox – New England often offer same-day assessments and next-day admission when clinically appropriate, helping you start care immediately. If you’re considering outpatient, our outpatient rehab programs explain what to expect.
Yes. MassHealth covers individual and group therapy at no cost, including psychiatric visits and family support. Coverage varies by plan, so it’s best to confirm. Our insurance verification team provides 24/7 reviews to give you a clear cost estimate before starting treatment.
Yes. Plymouth hosts Spanish- and Portuguese-language groups, and interpreters are available through the Massachusetts Behavioral Health Help Line. For clients seeking treatment with bilingual staff, Haven offers culturally responsive care and trauma-informed services.
Yes. Community centers and public programs provide sliding-scale fees, and the Massachusetts Health Safety Net can help cover essential care. Private providers like Haven offer detox, residential treatment, and dual diagnosis care with financial counseling and flexible payment plans.
Yes. GATRA transit connects residents to treatment centers, and programs like Taking People Places serve those with mobility needs. Haven Detox also coordinates transportation support to make admission seamless, especially for medical detox where urgent care is critical.
You can call the Massachusetts Behavioral Health Help Line at (833) 773-2445 or dial 988 for suicide prevention. For addiction-related emergencies, Haven offers 24/7 admissions and stabilization through its alcohol detox and drug detox programs.
Yes. Al-Anon meetings and family peer specialists in Plymouth offer confidential coaching. Haven also provides family therapy to strengthen communication and help families encourage their loved ones into treatment.
Programs across Plymouth provide Spanish-language, Portuguese, LGBTQ+-affirming, and faith-based services. Haven enhances this by offering trauma therapy and culturally responsive treatment options tailored to diverse communities in Massachusetts.
Yes. Community programs like Plymouth Recovery Center support young adults, and private facilities like Haven offer young adult rehab programs with peer recovery coaching, academic support, and relapse-prevention planning.
The Haven Detox provides insurance verification within 24 hours, plus sliding-scale payment options and advocacy for prior authorizations or appeals. This ensures you can still access care without unnecessary financial barriers.
Interface Referral Service: 888-244-6843
Serves Plymouth residents free of charge by connecting uninsured individuals to outpatient mental health providers and sliding-scale therapy options.
PCO Hope Community Outreach: 508-261-5488
Provides mobile crisis support for high-risk individuals through community-based harm reduction services, naloxone distribution, and peer recovery coaching.
Massachusetts Department of Public Health. Number of Opioid-Related Overdose Deaths by City/Town, 2016–2023. Boston, MA: MDPH; June 2024. Accessed September 12, 2025. https://www.mass.gov/doc/opioid-related-overdose-deaths-by-city-or-town-june-2024/download
Massachusetts Department of Public Health. Massachusetts opioid-related overdose deaths rose 2.5 percent in 2022 [press release]. Boston, MA: MDPH; June 22, 2023. Accessed September 12, 2025. https://www.mass.gov/news/massachusetts-opioid-related-overdose-deaths-rose-25-percent-in-2022
Massachusetts Department of Public Health. Data Brief: Opioid-Related Overdose Deaths among Massachusetts Residents, Updated through March 31, 2024. Boston, MA: MDPH; June 2024. Accessed September 12, 2025. https://www.mass.gov/lists/current-overdose-data
Executive Office of Health and Human Services. Community Behavioral Health Centers (CBHCs). Boston, MA: EOHHS. Accessed September 12, 2025. https://www.mass.gov/community-behavioral-health-centers
Executive Office of Health and Human Services. Behavioral Health Help Line (BHHL). Boston, MA: EOHHS. Accessed September 12, 2025. https://www.mass.gov/info-details/behavioral-health-help-line-bhhl-faq
MassHealth. Managed Care Entity Bulletin 113: Elimination of Copayments. Boston, MA: MassHealth; April 2024. Accessed September 12, 2025. https://www.mass.gov/doc/managed-care-entity-bulletin-113-elimination-of-copays-0/download
MassHealth. Pharmacy Facts #224: Pharmacy Copay Changes Effective April 1, 2024. Boston, MA: MassHealth; March 29, 2024. Accessed September 12, 2025. https://www.mass.gov/doc/pharmacy-facts-224-march-29-2024-0/download
MassHealth. MassHealth Copayment Information for Members. Boston, MA: MassHealth. Accessed September 12, 2025. https://www.mass.gov/info-details/masshealth-copayment-information-for-members
Town of Plymouth. Behavioral Health Resources [PDF]. Plymouth, MA: Town of Plymouth. Accessed September 12, 2025. https://plymouth-ma.gov/520/Mental-Health-Resources
Massachusetts Department of Public Health. Results of the Massachusetts Youth Health Survey 2023. Boston, MA: MDPH; 2024. Accessed September 12, 2025. https://www.mass.gov/doc/results-of-the-massachusetts-youth-health-survey-2023/download
Massachusetts Department of Public Health. Massachusetts Youth Health Survey (MYHS) – Reports & Data Tables. Boston, MA: MDPH. Accessed September 12, 2025. https://www.mass.gov/lists/massachusetts-youth-health-survey-myhs
Centers for Disease Control and Prevention. Youth Risk Behavior Survey Data Summary & Trends Report: 2009–2019, Updated 2023 Results. Atlanta, GA: CDC; 2024. Accessed September 12, 2025. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!