Dr. Rostislav Ignatov, MD
Chief Medical Officer
Suboxone is a prescription medication for opioid use disorder that combines buprenorphine (to relieve withdrawal and cravings) with naloxone (to discourage misuse).
Both inpatient facilities and outpatient clinics often use Suboxone (buprenorphine + naloxone) over buprenorphine-only because it is familiar and has the naloxone as an extra safety measure to prevent abuse.
Table of Contents
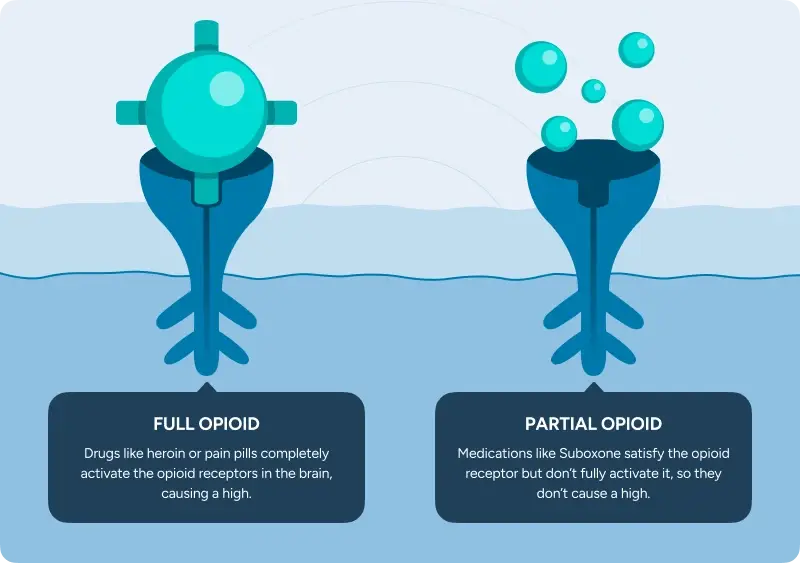
The buprenorphine in Suboxone attaches to the same opioid receptors in the brain that drugs like heroin, oxycodone and fentanyl attach to, but in a more controlled way that:
When Suboxone is taken correctly, naloxone has essentially no effect. Only a negligible amount can be absorbed under the tongue. If someone tries to misuse Suboxone by injecting it, the naloxone can block opioid effects and may cause sudden withdrawal symptoms. Since abusing Suboxone is likely to produce no high and potentially sickness, there is no incentive to misuse it.
Suboxone (buprenorphine) cannot be started too early!
The buprenorphine grabs opioid receptors very tightly and if there’s still a lot of heroin, oxycodone, or fentanyl actively affecting those receptors, buprenorphine can push them off too fast and cause precipitated withdrawal.
Precipitated withdrawal is often noted as 10/10 severe withdrawal symptoms that start very quickly (within minutes to a couple hours) after taking Suboxone too early.
It is primarily the buprenorphine (not the naloxone) that causes the precipitated withdrawals when Suboxone is taken under the tongue.
The Haven Detox staff typically wait until there are clear, objective signs of mild-to-moderate withdrawal, not just “I feel bad.”
A withdrawal scoring tool called the Clinical Opiate Withdrawal Scale (COWS) helps objectively analyze specific signs like:
There is not one exact amount of time that guarantees you will avoid precipitated withdrawal. Time can help as a rough guide, but symptoms and COWS score matter more.
With short-acting opioids (like heroin or immediate-release pills), withdrawal often shows up sooner so Suboxone may start as soon as 6-12 hours. Longer-acting opioids (like methadone) may be more like 24 to 72 hours. With drugs like fentanyl, timing is harder to predict.
In medical detox, the first dose is followed by reassessment. Many patients feel some relief after the first dose, but it may take a few adjustments to feel steady.
The goal is relief without over sedation, dizziness, or dangerously slowed breathing.
Patients are never left alone in withdrawal with 24/7 monitoring and a plan if symptoms spike. Other medications used during detox help with specific symptoms like stomach issues.
Many people start to feel some relief within 30 to 60 minutes of the first dose. For others, it can take a few careful dose adjustments over the first day to feel steady. Relief should feel like withdrawal is “turning down,” not like you’re sedated.
If fentanyl exposure is possible, The Haven Detox prefers to start with a low-dose initiation to ensure Suboxone is well tolerated before starting the full taper. This safer approach is not always standard protocol at other facilities and simply means:
Relief can take a little longer, but you avoid the severe sickness of precipitated withdrawal that typically feels worse.
| What “good relief” feels like | What “still under-dosed” can feel like | What “too much” can feel like |
| Less sweating, chills, yawning, and runny nose | Restless legs, pacing, or feeling unable to sit still | Very sleepy or hard to wake up |
| Fewer stomach cramps, less nausea, and less diarrhea | Ongoing nausea/diarrhea or stomach pain | Dizzy, lightheaded, or unsteady on your feet |
| Reduced anxiety and restlessness | Hot/cold flashes, goosebumps, watery eyes, runny nose | Confused or “out of it” |
| Cravings quiet down so you can rest, eat, and think more clearly | Strong cravings or a “crawling out of my skin” feeling | Slowed breathing |
| Trouble sleeping because symptoms keep breaking through |
The length of an opioid detox can vary a lot based on health and use history.
Generally:
If you’re staying in inpatient rehab after detox, you don’t have to rush off Suboxone. Whether you want to leave with a Suboxone prescription or not, you have more time to pace and plan a taper that works for you.

Some patients continue Suboxone after discharge for weeks to months (or longer) to help control cravings and stay stable.
If you have a history of overdose or chronic relapse, research and major healthcare organizations like SAMHSA and ASAM support the continued use of Suboxone. Ⓘ (We support you either way).
There is no shame in staying on medication that is helping you. The goal is safety, stability, and getting your life back.
No! Suboxone helps you to stabilize your life, which is the opposite of addiction.
As with many other medications, Suboxone involves physical dependence, but that is not the same as addiction.
Suboxone is designed to stabilize opioid receptors so it’s easier to focus on therapy, relationships, work, and day-to-day life. It has a “ceiling effect” that prevents a “high” and the naloxone discourages abuse.
If you’re worried about relapse or cravings, continuing Suboxone can be a great safety net.
The biggest risk most patients face is relapse. Detox lowers tolerance, so relapse can be more dangerous than before.
Suboxone is generally a helpful choice for most patients going through detox with opioid use disorder (OUD). A clinician may recommend a different plan if:
Major medical guidance supports treatment with Suboxone while pregnant, because untreated opioid use disorder during pregnancy carries serious risks. Historically, many providers preferred buprenorphine-only, but recent data reviewed by the American College of Obstetricians & Gynecologists (ACOG) found no adverse effects with Suboxone (buprenorphine/naloxone) in pregnancy. Ⓘ
Most side effects are manageable, especially when dosing is adjusted carefully, including:
Early in detox, it can be hard to tell what’s a medication side effect versus what’s still opioid withdrawal.
In a monitored setting, staff track when symptoms start (before or after a dose), check vital signs (heart rate, blood pressure, breathing), watch symptom patterns (like diarrhea vs constipation), and adjust the plan based on how you respond.
If side effects feel strong or don’t improve, the dose or timing may be changed and comfort medications can be added so symptoms don’t spiral.
Suboxone films and tablets dissolve in the mouth, creating a higher-risk environment for cavities, infections, and tooth loss.
To prevent dental issues from Suboxone:
Suboxone should be tapered down slowly under medical guidance. Stopping suddenly can cause withdrawal symptoms.
For most patients, Suboxone withdrawal is less intense, though it can last longer. A gradual taper keeps symptoms manageable and lowers the risk of relapse.
Patients at The Haven Detox decide with their team whether to stay on Suboxone for longer-term help or to be fully tapered while at detox.
Suboxone is generally much safer than illicit or full-opioid use, but it can be dangerous when mixed with other substances that slow breathing or cause heavy sedation, including:
In medical detox, staff review current prescriptions and substance use to reduce risks and monitor for oversedation. If continuing Suboxone after detox, ensure you understand the risks and take them seriously. Opioids are NOT going to have the effect you want, which is part of the deterrent.
Suboxone helps withdrawal and cravings, but people may still need symptom meds for sleep, nausea, diarrhea, and body aches, including:
Trying to push through opioid detox at home can turn dangerous fast.
Medical detox gives a much safer landing. Symptoms are treated, vitals are monitored, and the plan can be adjusted minute-by-minute.
Most insurance plans cover detox and the medications used (including Suboxone).
Get answers about your cost / coverage now.
Your information will be kept private
Let’s talk about what’s going on — no judgment. (We’ve been there before ourselves). No one will know you inquired and there is no commitment to call.
24/7 Support
No Commitment
100% Private
There’s no catch. Checking your insurance is simply a way to see what your plan covers — it doesn’t lock you into treatment, notify anyone, or cost you anything. You get answers upfront to decide what makes sense for you.
Protecting your privacy matters! No information or notifications are ever sent to your employer or family — whether you check your insurance online or call. Everything is handled through secure, encrypted systems that meet strict medical privacy laws. You stay in control of your information!
Luckily, most insurance policies cover treatment here. Depending on the healthcare you’ve already had this year, costs could even be zero. Instead of worrying, let’s just find out what your plan covers.
Most likely. We work with major providers like Cigna, Aetna, and United Healthcare, public insurances like Tricare and tribal plans, and even smaller plans like Surest Bind and Harvard Pilgrim. The quickest way to know for sure is to check online or call. It’s a quick, private way to understand what is covered upfront.
Verifying your insurance isn’t a commitment to start treatment — it’s simply a way to see what your options are. Knowing your coverage ahead of time helps you make more informed, confident decisions. It also helps flag a spot, so you’re able to get right in if you ever do decide you’re ready.
You need your policy number to check your specific policy online. If you want general information, just call. You likely have questions beyond insurance anyway. Reaching out now helps you figure out the right fit if or when you’re ready. You don’t have to put off the call until you’re in crisis. Calling is not scary, I promise!